All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Differences in organ damage accrual between African American and Caucasian patients with SLE
Do you know... The Systemic Lupus International Collaborating Clinics (SLICC)/revised American College of Rheumatology (ACR) classification criteria is a method for assessing organ damage in patients with SLE. In a study by Kallas, et al., which organ system showed a significantly higher SLICC/ACR damage index in African American patients compared to Caucasian patients with SLE?
Organ damage is a significant issue for patients with systemic lupus erythematosus (SLE) and patients who accrue damage early have a poorer prognosis, with organ damage in the first year being associated with a 3–4-fold increase in 10-year mortality.1
The role of ethnicity and socioeconomic status in the pattern and severity of damage accrual in SLE has been unclear, with few studies examining these areas together. To address this, Kallas and colleagues1 published an article in Journal of Rheumatology, which examines the trajectory of damage accrual overall and in individual organ systems in a group of African American and Caucasian patients with SLE, including an assessment of the impact of specific socioeconomic factors. We are pleased to provide a summary of this article here.
Study design
The study included 2,436 patients with SLE divided into two cohorts based on ethnicity from the prospective Hopkins Lupus Cohort, who were classified using the Systemic Lupus International Collaborating Clinics (SLICC) classification criteria or revised American College of Rheumatology (ACR) classification criteria.
The SLICC/ACR damage index (DI) includes 12 organ systems to measure damage, which is defined as “irreversible organ dysfunction, present for 6 months or longer regardless of etiology” and was used to compare the DI between the two groups.
Socioeconomic factors were collected by self-reported patient questionnaires and included years of education, insurance type, and combined family income.
Results
Patient characteristics
In the overall cohort, 42.9% of patients were African American and 57.1% were Caucasian and the mean age when SLE was diagnosed was 33 years. Patients diagnosed with SLE before the age of 30 years made up 49% of the overall cohort, with 33.6% being diagnosed when aged 30−45 years.
As shown in Table 1, the groups comprising African American and Caucasian patients were well-matched with regards to age, follow-up time since diagnosis, and sex. When looking at socioeconomic markers, African American patients were less likely to have >12 years of education, a household income of >$65,000, or to have private health insurance compared with Caucasian patients.
Table 1. Baseline patient characteristics*
|
SD, standard deviation; SLE, systemic lupus erythematosus. |
|||
|
Baseline characteristic, % (unless otherwise stated) |
All |
African American |
Caucasian |
|---|---|---|---|
|
Mean age at SLE diagnosis ± SD, years |
32.7 ± 13.0 |
31.3 ± 12.1 |
33.6 ± 13.5 |
|
Mean follow-up since SLE diagnosis ± SD, years |
13.4 ± 10.0 |
13.6 ± 10.2 |
13.3 ± 9.8 |
|
Female |
92 |
93.4 |
91.0 |
|
Education |
|
|
|
|
≤12 years |
34 |
40.8 |
28.7 |
|
>12 years |
66 |
59.2 |
71.3 |
|
Family income |
|
|
|
|
<$30,000 |
33 |
49.2 |
20.3 |
|
$30,000 − <$65,000 |
33 |
28.9 |
35.8 |
|
≥$65,000 |
24 |
21.8 |
43.9 |
|
Insurance |
|
|
|
|
None |
2 |
4.0 |
1.3 |
|
Medical assistance |
19 |
30.2 |
10.9 |
|
Private |
78 |
65.8 |
87.8 |
Association between ethnicity and damage accrual in organ systems
The organ systems that showed a significant difference between the two patient groups in terms of damage accrual are shown in Table 2. Following adjustments for sex, age at diagnosis, years of education, health insurance, and household income, African American patients were shown to have a significantly higher rate of damage accrual compared with Caucasian patients. This was particularly notable in the renal and pulmonary systems and the skin.
On univariate analysis, there was also a significant difference in risk of musculoskeletal and cardiovascular damage, but this was not significant following adjustment for age at diagnosis, sex, and socioeconomic factors.
Table 2. Adjusted and unadjusted rates of damage accrual in African American and Caucasian patients in organ systems*
|
CI, confidence interval; SLICC/ACR DI, Systemic Lupus International Collaborating Clinic/revised American College of Rheumatology damage index. |
||||||
|
Type of damage |
Rate of SLICC/ACR DI per year |
Rate ratio |
p value |
Adjusted rate ratio† |
p value |
|
|---|---|---|---|---|---|---|
|
African American |
Caucasian |
|||||
|
Total |
0.16 |
0.12 |
1.30 |
<0.0001 |
1.14 |
0.010 |
|
Renal |
0.03 |
0.016 |
1.99 |
<0.0001 |
1.68 |
<0.0001 |
|
Pulmonary |
0.016 |
0.011 |
1.47 |
0.0006 |
1.38 |
0.0066 |
|
Cardiovascular |
0.012 |
0.009 |
1.32 |
0.0352 |
1.26 |
0.1023 |
|
Musculoskeletal |
0.03 |
0.02 |
1.31 |
0.0002 |
1.11 |
0.2086 |
|
Skin |
0.007 |
0.002 |
4.15 |
<0.0001 |
2.98 (1.83–4.85) |
<0.0001 |
Association between ethnicity and individual damage items
The association between individual DI items according to SLICC/ACR is shown in Figure 1 and indicates that African American patients had an increased adjusted rate ratio for the following compared with Caucasian patients at any time during follow-up:
- Renal insufficiency
- Proteinuria 3.5 g/24 hours
- End-stage renal disease
- Pulmonary hypertension
- Pulmonary fibrosis
- Cardiomyopathy
- Pericarditis
- Deforming or erosive arthritis
- Avascular necrosis
- Scarring chronic alopecia
Additionally, there were specific SLICC/ACR DI items that were increased in Caucasian patients, including osteoporosis with fracture or vertebral collapse, bowel infarction, venous thrombosis, and malignancy.
Figure 1. Forest plot showing the SLICC/ACR DI items that were significantly different between ethnic groups*
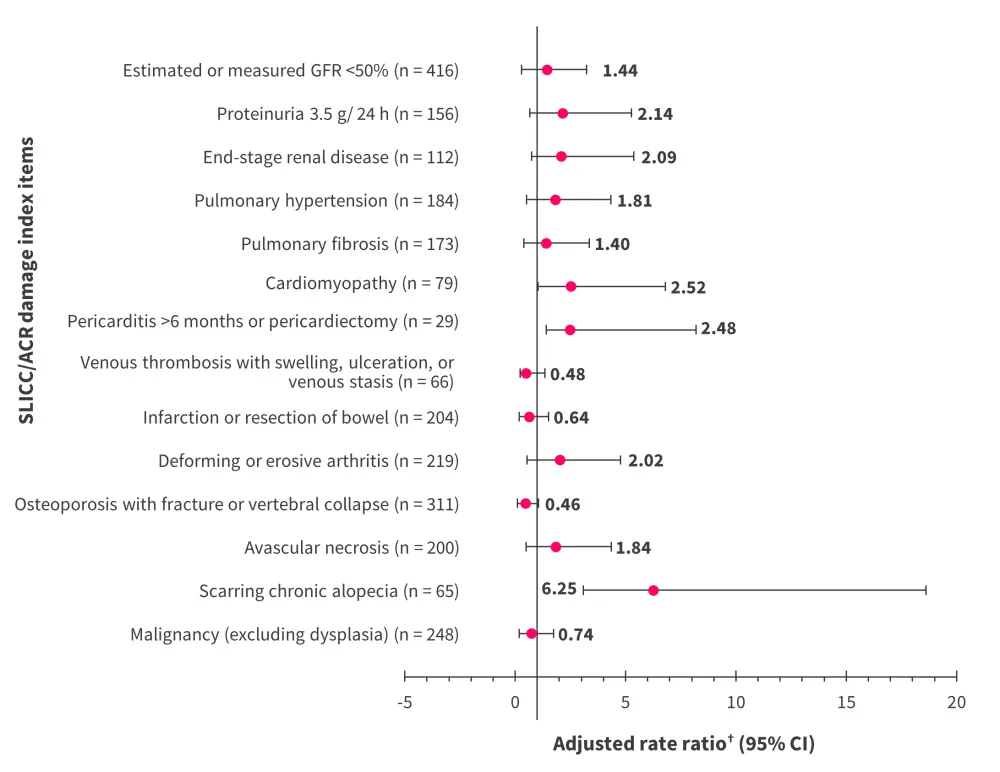
ACR, American College of Rheumatology; GFR, glomerular filtration rate; SLICC, Systemic Lupus International Collaborating Clinics.
*Data from Kallas, et al.1
†Adjusted for sex, age at diagnosis, years of education, income, and insurance.
Association between ethnicity and damage accrual in organ systems over time
Assessing trends in damage accrual over time showed a linear increase for both groups of patients with SLE. Increased mean damage scores for skin and renal, pulmonary, and musculoskeletal systems were observed in African American patients compared with Caucasian patients at any point following SLE diagnosis. The incidence of damage in specific organ systems is shown in Table 3.
Table 3. Incidence of damage in specific organ systems over time*
|
SLE, systemic lupus erythematosus. |
||
|
Incidence, % |
African Americans |
Caucasians |
|---|---|---|
|
5 years after SLE diagnosis |
|
|
|
Incidence of renal damage |
11 |
6 |
|
15 years after SLE diagnosis |
|
|
|
Incidence of renal damage |
21 |
14 |
|
Incidence of pulmonary damage |
17 |
14 |
|
Incidence of musculoskeletal damage |
35 |
25 |
|
Incidence of skin damage |
11 |
3 |
Conclusion
There were certain limitations to the study; socioeconomic factors were considered to be fixed following SLE diagnosis, the individual impact of the three measures of socioeconomic status could not be analyzed individually, and confounding variables, such as disease activity, corticosteroid use, adherence to medication, and obesity, were not accounted for. In addition, this study was predominantly focused on African American and Caucasian patients so its findings cannot be generalized to other ethnicities.
On the other hand, the study had certain strengths. The large cohort of patients from two ethnic groups was followed-up for a mean of 13 years. In addition, the impact of socioeconomic status was assessed with three different measures.
The study showed that African American patients with SLE not only are more likely to experience damage accrual in their renal, pulmonary, or skin systems but that it occurs at a faster rate compared with Caucasian patients even after adjusting for socioeconomic factors. Therefore, in this study, ethnicity was a significant factor in organ damage severity, rate of accrual, and the organ systems affected in patients with SLE. Both Caucasian and African American patients showed a linear increase in damage over time, which shows the need for interventions to protect against organ damage.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

