All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
The association of race and ethnicity with COVID-19 outcomes in patients with SLE
Do you know... In an analysis of the COVID-19 Global Rheumatology Alliance registry between March 24, 2020, and August 27, 2021, what percentage of Black patients with SLE were hospitalized but did not require oxygenation after the development of COVID-19?
Differing rates of morbidity and mortality have been reported following infection with SARS-CoV-2 in people from different races and ethnicities, with Black and Hispanic patients often experiencing worse outcomes compared with White patients.1 Patients with systemic lupus erythematosus (SLE) who are non-White also show more severe SLE symptoms and have a higher mortality rate.1
The impact of the COVID-19 pandemic on patients with SLE of different race and ethnicity has not been previously assessed in the US.1 In this article we summarize a paper by Manuel Ugarte-Gil, et al.1, published in Arthritis Care Research, on the association between race and ethnicity and COVID‑19 outcomes in patients with SLE.
Study design
Patients with SLE and COVID-19 who were added to the COVID-19 Global Rheumatology Alliance (C19-GRA) registry between March 24, 2020, and August 27, 2021, were included in the study. Data on the race and ethnicity of the patient was entered by the physician treating each case.
COVID-19 outcomes were split into the following four categories:
- Not hospitalized
- Hospitalized with no oxygenation
- Hospitalized with any ventilation or oxygenation
- Death
Results
Results from 469 patients with SLE were included in this study and the baseline characteristics are shown in Table 1. Of the patients included on this study, 90.6% were female, the mean age was 46.4 years, 34.3% were White, 26.9% were Black, 32.8% were Hispanic, and 6% were other/mixed. White patients had a higher mean age of 50.4 years, but a lower number of comorbidities (50.3% had 0) compared with the other groups.
The majority of patients were classed as having disease activity that was minimal or low (58.4%) and 55.7% had ≥1 comorbidity.
Table 1. Baseline patient characteristics*
|
CVD, cardiovascular disease; ESRD, end-stage renal disease; SD, standard deviation; SLE, Systemic lupus erythematosus. |
|||||
|
Characteristic, % (unless otherwise stated) |
Total† |
White |
Black |
Hispanic |
Other/ mixed |
|---|---|---|---|---|---|
|
Mean age, years (SD) |
46.4 (13.7) |
50.4 (14.5) |
45.8 (13.1) |
43.2 (12.0) |
42.9 (15.2) |
|
Female |
90.6 |
91.3 |
92.1 |
89.6 |
85.7 |
|
Date of COVID-19 diagnosis |
|
|
|
|
|
|
Prior to Jun 15, 2020 |
39.2 |
32.3 |
57.9 |
32.5 |
32.1 |
|
Jun 16, 2020, to Sep 30, 2020 |
14.7 |
11.8 |
16.7 |
17.5 |
7.1 |
|
Oct 1, 2020, to Aug 27, 2021 |
46.1 |
55.9 |
25.4 |
50.0 |
60.7 |
|
Comorbidities |
|
|
|
|
|
|
0 |
44.4 |
50.3 |
38.1 |
43.5 |
42.9 |
|
1 |
33.9 |
34.2 |
34.1 |
33.1 |
35.7 |
|
≥2 |
21.8 |
15.5 |
27.8 |
23.4 |
21.4 |
|
Specific comorbidities |
|
|
|
|
|
|
Chronic renal insufficiency or |
13.7 |
6.2 |
15.9 |
16.2 |
32.1 |
|
Hypertension or CVD |
36.7 |
31.7 |
46.0 |
35.1 |
32.1 |
|
Disease activity |
|
|
|
|
|
|
Remission |
20.7 |
23.6 |
17.5 |
20.1 |
21.4 |
|
Minimal or low |
58.4 |
57.8 |
63.5 |
55.8 |
53.6 |
|
Moderate |
15.1 |
11.8 |
12.7 |
19.5 |
21.4 |
|
Severe or high |
2.1 |
1.9 |
4.0 |
1.3 |
0.0 |
|
Missing |
3.6 |
5.0 |
2.4 |
3.3 |
3.6 |
The COVID-19 outcomes, split between the different racial and ethnic groups, are shown in Figure 1. White patients with SLE and COVID-19 were not hospitalized in 86.3% of cases, whereas only 63.5% of Black patients were not admitted. Black patients showed the highest percentage of patients hospitalized without requiring ventilation, at 14.3%.
Black and Hispanic patients were the most likely to require ventilation or oxygenation in hospital (both 17.5%) compared with White or other/mixed patients. In addition, 4.8% of Black patients died, compared with 3.9% of Hispanic patients, 3.6% of other/mixed patients, and 3.1% of White patients, who had the lowest fatality rate.
Figure 1. COVID-19 outcomes*
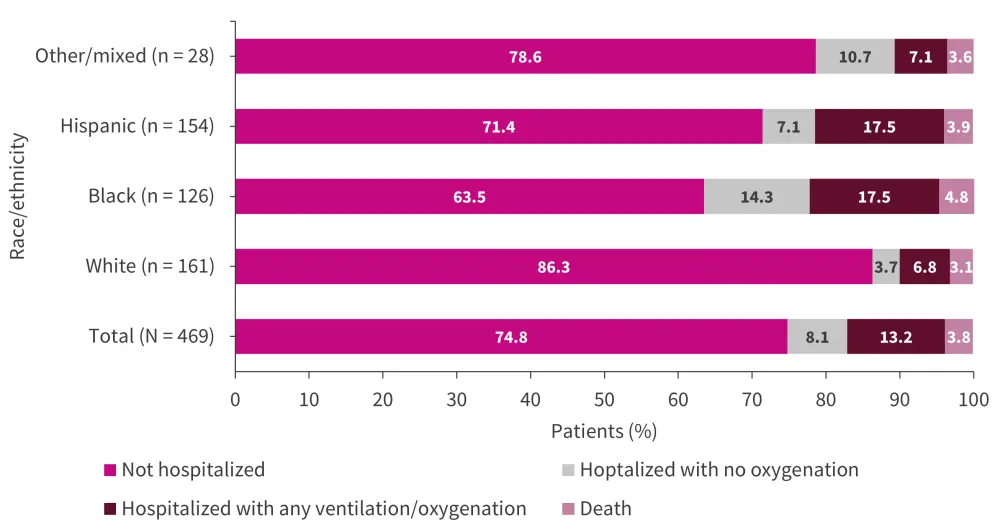
*Adapted from Ugarte-Gil, et al.1
Multivariate analysis carried out on the COVID-19 outcome data showed that Black and Hispanic patients had significantly increased odds ratios for severe outcomes compared with White patients (Table 3). Patients who were Black also showed a significantly increased odds ratio for being hospitalized compared with White patients.
Table 3. Multivariate analysis of the association between race/ethnicity and COVID-19 outcomes in patients with SLE in the US*
|
CI, cumulative incidence; OR, odds ratio. |
||||
|
Race/ethnicity |
Ordinal outcome† |
Hospitalization |
||
|---|---|---|---|---|
|
OR (95% CI) |
p value |
OR (95% CI) |
p-value |
|
|
White |
Ref |
|
Ref |
|
|
Black |
2.73 (1.36–5.53) |
<0.01 |
2.15 (1.16–3.99) |
0.02 |
|
Hispanic |
2.76 (1.34–5.69) |
<0.01 |
1.73 (0.94–3.16) |
0.08 |
|
Other |
1.13 (0.34–3.77) |
0.85 |
1.22 (0.42–3.49) |
0.71 |
Limitations
As the C19-GRA registry used was one that collected data reported by physicians, the results may have been biased to include more severe cases, as these were more likely to seek medical help. Other selection biases may also exist, such as differences in access to healthcare. This study did not take into account confounding variables, such as poverty, and other issues that may underlie the disparities in health outcomes in the US. These data are from the US and may not be generalizable to other countries. Race and ethnicity were entered by the attending physician and may not have been entered in accordance with the ethnicity the patient self-identified as. In addition, some variables assessed had small patient numbers, so the outcomes assessed should be treated with caution.
The impact of vaccination on outcome was not analyzed in this study, as the majority of cases were recorded prior to the availability of any of the COVID-19 vaccines.
Conclusion
Black and Hispanic patients with SLE have been reported to have more severe SLE symptoms and a higher mortality rate in the US. In addition, Black or Hispanic individuals without SLE also demonstrate poorer outcomes following cases of COVID-19 in the US. This trend continues when examining the association between race and ethnicity and COVID-19 outcome, with Black and Hispanic patients with SLE faring worse compared with White patients. The authors of this study attributed this association to socioeconomic factors and inequality when accessing healthcare.
Black and Hispanic patients with SLE showed worse post-COVID-19 outcomes than white patients in the US. This result may reflect the inequality in access to healthcare for Black and Hispanic patients, who are more likely to be from a poorer socioeconomic background and have fewer healthcare services locally available to them.
Expert Opinion
Manuel Ugarte-Gil provides his expert opinion on how race/ethnicity and COVID-19 outcomes in patients with SLE in the US relate to clinical practice:
“This study reinforces the relevance of socioeconomic characteristics in the outcomes of patients with SLE; patients from a low socioeconomic status are less likely to be able to work from home (telework) and more likely to have limited access to the healthcare system, both resulting in poorer outcomes. Furthermore, health literacy and trust in the healthcare system and on its providers, have been reported to be lower in non-White populations, reflecting oftentimes structural racism. To reduce the outcome gaps observed, we must actively work on reducing disparities, for example by improving educational activities considering the differences between these groups.”
 Manuel Francisco Ugarte-Gil
Manuel Francisco Ugarte-GilReferences
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

