All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
A summary of a prospective cohort study that compared the effects of attaining LLDAS in patients with newly diagnosed SLE versus established SLE
Do you know... In a recent multicenter, prospective study comparing the effects of lupus low disease activity state LLDAS attainment in patients with newly diagnosed versus established SLE, which of the following parameters was significantly higher in patients with newly diagnosed SLE?
Systemic lupus erythematosus (SLE) is associated with a significant impact on health-related quality of life (HR-QoL) and until now there has been a lack of measures of treatment outcome status for use in clinical trials.1
Lupus low disease activity state (LLDAS), a measure that combines disease activity and treatment domains, is a prospectively validated treat-to-target strategy.1 Prospective and retrospective studies show that attainment of LLDAS is associated with better HR-QoL and offers a protective effect against flares, damage accrual, and mortality.1-3 However, these studies included only patients with established SLE, therefore, skewing the results and warranting investigation of the effects of LLDAS in patients with newly diagnosed SLE.
During the European Alliance of Associations for Rheumatology (EULAR) 2022 Congress, Eric Morand, Monash University, Melbourne, AU, presented the findings from a multicenter, prospective study comparing the effects of LLDAS attainment in patients with newly diagnosed versus established SLE.4 The key findings are summarized here.
Study design
This was a prospective, multicenter, cohort study conducted between May 2013 and December 2020 in patients aged ≥18 years and diagnosed with SLE using American College of Rheumatology (ACR) or Systemic Lupus International Collaborating Clinics (SLICC) criteria. As shown in Figure 1, patients were divided into two cohorts: the inception cohort in which the patients were enrolled <1 year since the onset of SLE (n = 680) and the non-inception cohort in which the patients were enrolled >1 year since the onset of SLE (n = 3,426).
At 3–6 months, data were collected on:
- Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) score;
- Physician Global Assessment (PGA) score;
- medicine use, including prednisolone dose; and
- clinical parameters.
The outcome measures included
- flare assessment (at every visit);
- damage accrual (yearly); and
- HR-QoL (yearly).
Figure 1. The inception and non-inception cohorts over the 5-year follow-up*
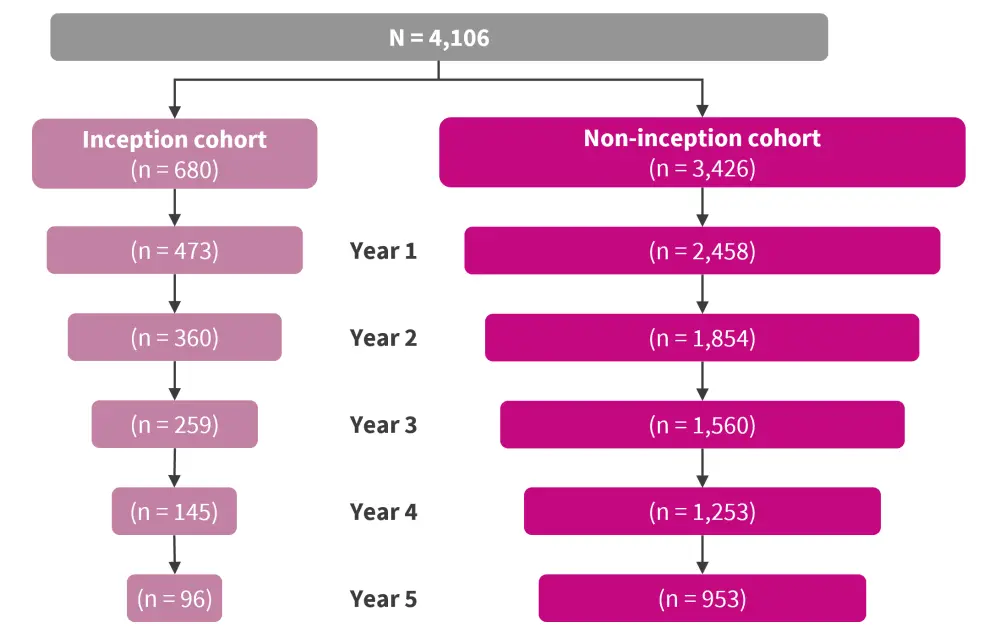
*Adapted from Morand.4
Results
Baseline characteristics
A total of 4,106 patients were included, with 680 and 3,426 patients in the inception and non-inception cohorts, respectively. Patients in the inception cohort were younger, showed more active disease, had higher prednisolone use, were less likely to be in LLDAS, and had less damage accrual at enrolment (Table 1). Only 13.6% of patients in the inception cohort accrued damage during a median follow-up of 2.2 years.
Table 1. Characteristics of the inception and non-inception cohorts*
|
AMS, adjusted mean SLEDAI-2K; IQR, interquartile range; LLDAS, lupus low disease activity state; PNL, prednisolone; PGA, Physician Global Assessment; SLE, systemic lupus erythematosus; SLEDAI-2K, Systemic Lupus Erythematosus Disease Activity Index 2000; TAM, time-adjusted mean. |
|||
|
Characteristic |
Inception cohort |
Non-inception cohort |
p value |
|---|---|---|---|
|
Median age, years (IQR) |
33.0 (25.0–44.0) |
40.0 (31.0–51.0) |
<0.001 |
|
Median SLE duration at enrollment, years (IQR) |
1.0 (0.0–1.0) |
10.0 (5.0–16.0) |
<0.001 |
|
Median study duration, years (IQR) |
2.2 (0.9–3.7) |
2.5 (1.0–5.4) |
<0.001 |
|
PNL use ever, % |
91.2 |
83.6 |
<0.001 |
|
Median TAM-PNL (IQR) |
6.2 (3.2–10.3) |
5.0 (2.2–8.6) |
<0.001 |
|
Median AMS (TAM-SLEDAI-2K) (IQR) |
3.1 (1.6–5.0) |
2.8 (1.2–4.6) |
0.002 |
|
Median TAM-PGA (IQR) |
0.4 (0.3–0.8) |
0.4 (0.2–0.7) |
<0.001 |
|
Flare ever, % |
57.5 |
52.2 |
0.012 |
|
Baseline organ damage, % |
25.7 |
40.9 |
<0.001 |
|
Organ damage accrual, % |
13.6 |
20.8 |
<0.001 |
|
LLDAS at baseline, % |
28.7 |
50.5 |
<0.001 |
|
LLDAS ever (at least once), % |
73.9 |
78.2 |
0.014 |
|
≥50% cumulative time in LLDAS, % |
41.1 |
50.6 |
<0.001 |
|
≥3 months in sustained LLDAS, % |
51.8 |
57.2 |
0.009 |
Lupus low disease activity state
At enrolment, significantly fewer patients were in LLDAS in the inception cohort compared with the non-inception cohort (28.7% vs 50.5%; p < 0.001). LLDAS was achieved at least once during follow-up by a lesser percentage of patients in the inception cohort compared with the non-inception cohort, at 73.9% and 78.2%, respectively. Limiting analysis only to patients who did not attain LLDAS at enrolment, time to first LLDAS attainment was significantly higher in the inception cohort compared with the non-inception cohort (hazard ratio, 1.60, 95% confidence interval, 1.40–1.82; p < 0.001).
Protective effect
A protective effect of LLDAS against flares was observed in both the inception and non-inception cohorts. In the inception cohort, in patients who had ever attained LLDAS, the protective effect against flares was statistically significant (p < 0.001). However, no significant association was observed for the protective effect against damage accrual in the inception cohort (p = 0.254) (Figure 2).
Figure 2. Protective effect of LLDAS against flares and damage accrual*
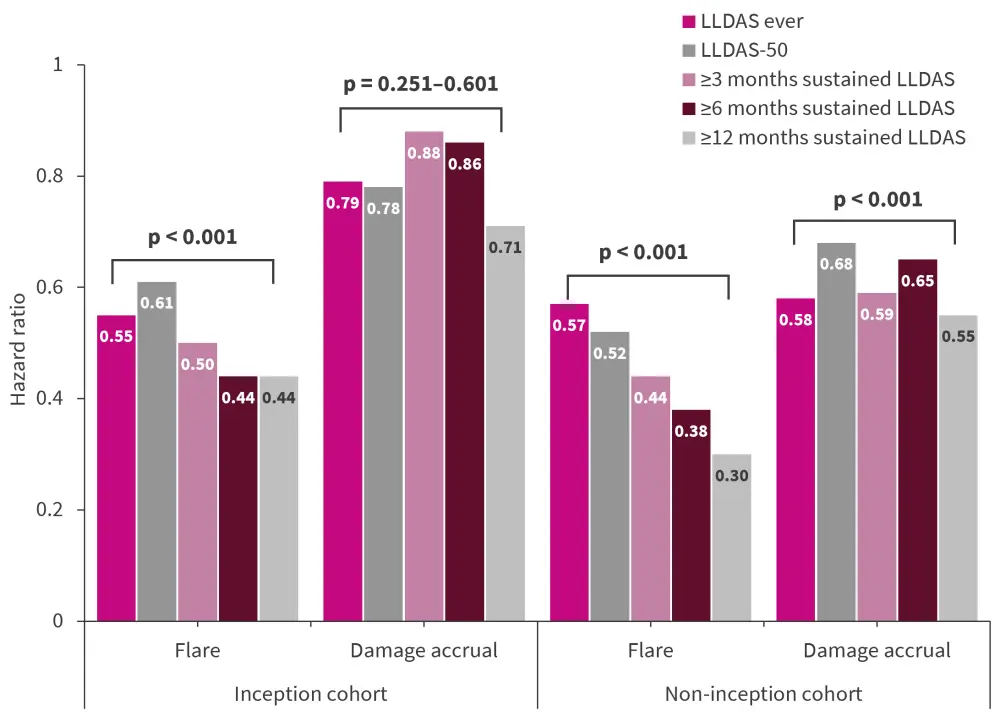
LLDAS, lupus low disease activity state; LLDAS-50, LLDAS ≥50%.
*Data from Morand.4
Conclusion
This prospective cohort study demonstrated that time to first LLDAS attainment from baseline was shorter in the inception cohort, suggesting that LLDAS could be applied as a treat-to-target strategy at diagnosis in patients with newly diagnosed SLE. The attainment of LLDAS also showed a protective effect against flares in patients with recent onset of SLE (the inception cohort). However, there was no significant protection against damage accrual in this population mainly due to low rates of damage accrual in the first years after SLE diagnosis. Further long-term follow-up is therefore needed to establish if LLDAS offers a protective effect against damage accrual in patients with newly diagnosed SLE. Some other limitations of the study included variation in the definition of the inception cohort and change in disease activity in patients during the study period.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

