All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Anifrolumab treatment in adolescents with recalcitrant discoid lupus erythematosus: a case series
Context
Anifrolumab has emerged as a promising treatment option for refractory discoid lupus erythematosus (DLE), following its 2021 approval for adults with systemic lupus erythematosus (SLE). However, its effectiveness in treating adolescents with SLE and recalcitrant DLE is unclear. Here, we summarize a case series published by Shaw et al.1 in JAMA Network Open on the effectiveness and safety of anifrolumab in recalcitrant adolescents with DLE.
Methods
This multicenter, retrospective case series included adolescents with SLE and recalcitrant DLE treated between August 1, 2022, and June 30, 2023. The primary outcome was reduction in Cutaneous Lupus Erythematosus Disease Area and Severity Index score (CLASI)-Activity (CLASI-A) score and CLASI-Damage (CLASI-D).
Key findings
The case series included seven adolescents with DLE with a median age of 17 years (range, 14–20 years), treated intravenously with 300 mg anifrolumab every 4 weeks. Four patients were Asian, two were Black/African American, and one patient was White. The baseline characteristics are presented in Figure 1.
Figure 1. Baseline characteristics, current treatment regimen, and outcomes*
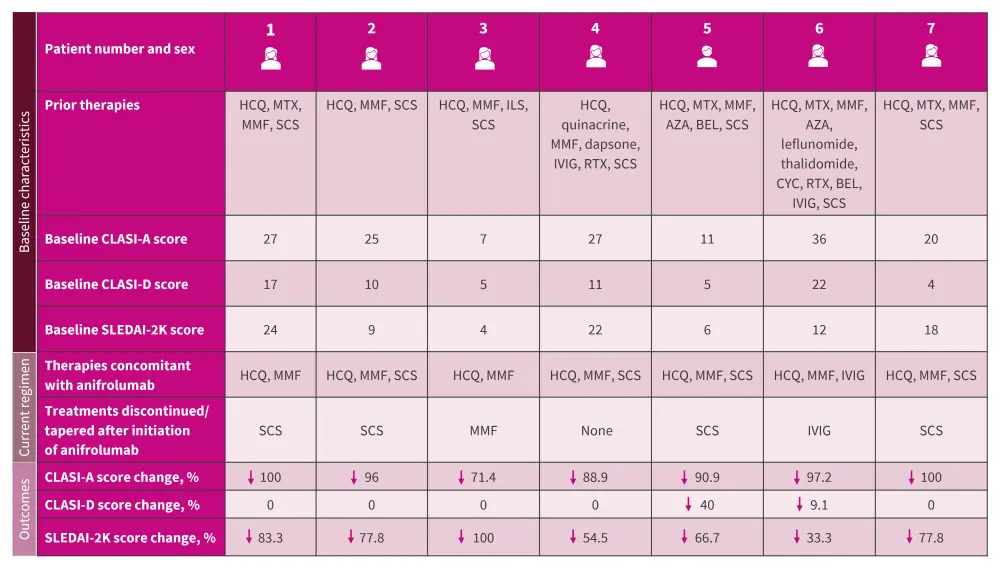
AZA, azathioprine, BEL, belimumab; HCQ, hydroxychloroquine; CLASI-A, Cutaneous Lupus Erythematosus Disease Area and Severity Index–Activity; CLASI-D, CLASI–Damage; IVIG, intravenous immunoglobulin; ILS, intralesional corticosteroids; MMF, mycophenolate mofetil; MTX, methotrexate; RTX, rituximab; SLEDAI-2K, Systemic Lupus Erythematosus Disease Activity Index 2000; SCS, systemic corticosteroid.
*Data from Shaw, et al.1
A substantial improvement in cutaneous disease activity was observed in all patients initiating anifrolumab. Within a month of initiation, a 72.1% mean decrease in CLASI-A score was reported (p = 0.01); this sustained at 6-month follow-up. There was an improvement in overall disease activity, measured by SLE Disease Activity Index 2000 score, with a mean decrease of 7.0 at the last follow-up. The CLASI-D scores calculated at Month 1 and 6 showed no significant differences compared with baseline.
Anifrolumab was well tolerated. One case of recurrent herpes simplex virus type 1 reactivation was reported, in line with the increased susceptibility to viral infections noted in clinical trials, as previously published on the Lupus Hub.
Key learnings
The findings indicate that anifrolumab induces rapid and persistent responses in adolescents with DLE for whom conventional therapies fail to yield a response. The study limitations include its retrospective design and relatively small patient population.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

