All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Association between glucocorticoids and chronic damage accrual in patients with SLE
Do you know... Achievement of GC-free status is associated with less chronic damage. In the study by Sada et al., no significant difference was found in GC-free status in patients with or without chronic damage in which disease durations?
Glucocorticoids (GCs) are one on the main treatments for patients with systemic lupus erythematosus (SLE), despite previous studies linking GC use with chronic damage accrual in these patients. GC use is still high due to the increased risk of relapse in SLE patients resulting from withdrawal; however, studies have shown that 73–85% of patients could maintain remission without GCs.
Chronic damage in SLE patients can lead to a reduced quality of life and increased mortality risk. Here, we summarize a study by Sada et al.,1 recently published in Lupus Science & Medicine, investigating the factors associated with a GC-free treatment status in SLE patients.
Study design
Data was gathered from the lupus registry of nationwide institutions (LUNA), which contains data from SLE patients across ten Japanese institutions, through questionnaires or electronic medical records between 2016 and 2020. Only patients with known GC dose data were enrolled. Figure 1 shows the GC doses that patients were receiving at registration.
Figure 1. GC dosing at registration*
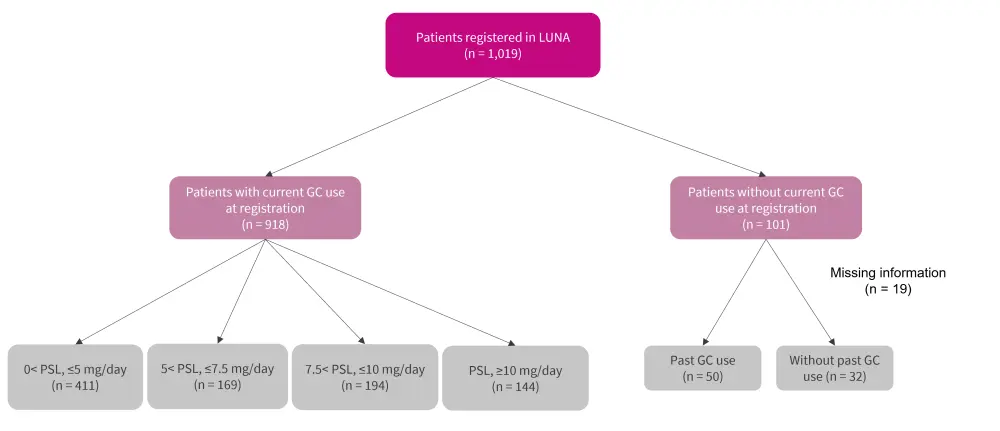
GC, glucocorticoid; PSL, prednisolone.
*Adapted from Sada, et al.1
Results
Baseline patient characteristics of the 1,019 enrolled patients are given in Table 1. The majority of patients were female, with a higher percentage of patients who had been treated with GCs also using immunosuppressants and/or hydroxychloroquine at the time of registration, compared with patients who had never been treated with GCs. Also, Patients never treated with GCs were older than patients treated with GCs.
Table 1. Baseline patient characteristics*
|
ds, double stranded; GC, glucocorticoid; IQR, interquartile range; SLEDAI-2K, SLE Disease Activity Index 2000; SLICC-DI, Systemic Lupus International Collaborating Clinics Damage Index. |
|||||
|
Characteristic, % |
Patients never |
Number of |
Patients |
Number of |
p value |
|---|---|---|---|---|---|
|
Median age (IQR), |
50.5 (40.8– |
0 |
44.5 (32–56) |
0 |
0.012 |
|
Female |
84 |
0 |
88 |
0 |
0.41 |
|
Median disease |
13 (6–22.5) |
1 |
12 (6–20) |
20 |
0.41 |
|
<5 years |
22 |
0 |
25 |
0 |
|
|
5–20 years |
47 |
0 |
50 |
0 |
|
|
≥20 years |
31 |
0 |
26 |
0 |
|
|
Median SLEDAI-2K |
2 (0–6) |
9 |
4 |
223 |
0.027 |
|
Median SLICC-DI |
0 (0–2) |
0 |
1 (0–2) |
0 |
0.61 |
|
Median maximum |
50 (30-60) |
0 |
40 (30-50) |
70 |
0.48 |
|
Current |
42 |
0 |
65 |
0 |
0.0010 |
|
Current |
4 |
0 |
29 |
0 |
<0.0001 |
|
Median anti-ds-DNA |
7.6 (1.7–10.1) |
3 |
9.15 (2.4–20.8) |
24 |
0.23 |
|
Serum creatinine |
0.66 (0.60– |
1 |
0.69 (0.59– |
2 |
0.31 |
Disease duration and other treatments
Shorter disease duration was more commonly seen in patients not currently using GCs. Of these patients, 66% had short duration, 23% had middle duration, and 17% had long duration (p = 0.00029). Patients with longer disease duration were less likely to be treated with immunosuppressants and hydroxychloroquine than patients with other disease durations (Figure 2).
Figure 2. Use of immunosuppressants and hydroxychloroquine in different disease durations*
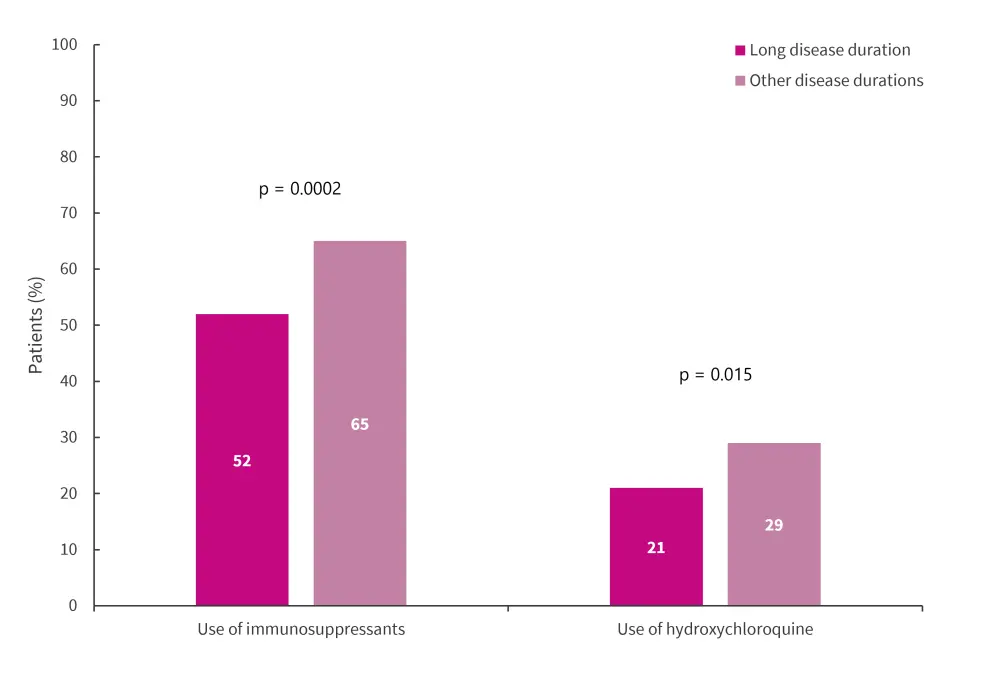
*Adapted from Sada, et al.1
GC-free status and chronic damage accrual and disease duration
GC-free treatment status was more often associated with no chronic damage accrual (a Systemic Lupus International Collaborating Clinics Damage Index [SLICC-DI] of 0) when compared with patients who had chronic damage accrual and a long disease duration (11% vs 4%; p = 0.023). The percentage of patients achieving SLICC-DI for different organs varied across disease durations, with occular, renal, cardiovascular, peripheral vascular, musculoskeletal, and diabetic impairments increasing with disease duration (Figure 3).
Figure 3. Patients achieving SLICC-DI for organs across different disease durations*
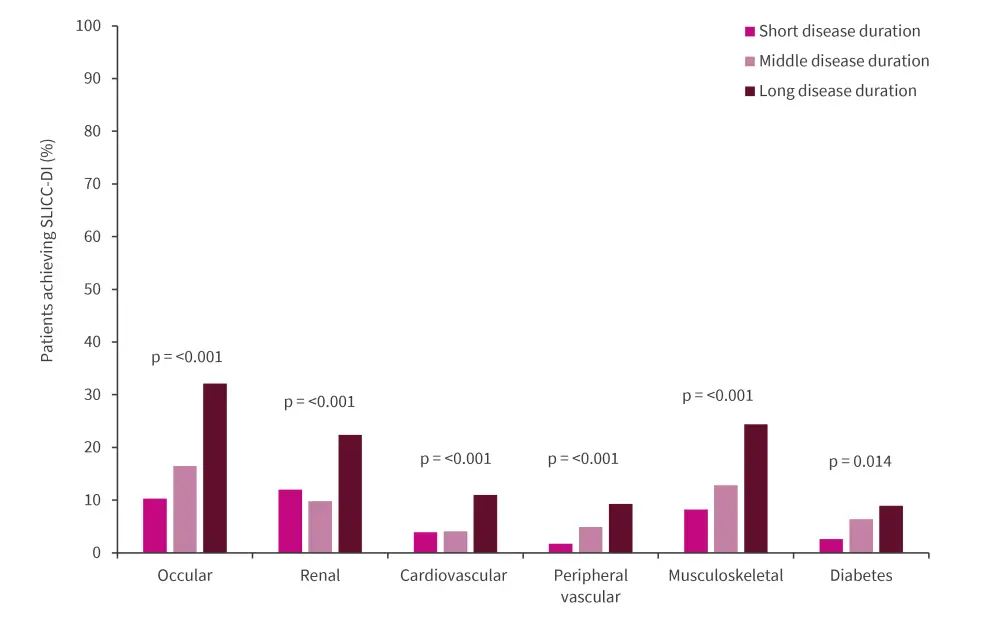
SLICC-DI, Systemic Lupus International Collaborating Clinics Damage Index.
*Adapted from Sada, et al.1
Absense of chronic damage was associated with a GC-free treatment status, even when adjustments were made for other factors including age, sex, and a disease duration of ≥20 years. Sada et al. found no significant difference in GC-free status in patients with or without chronic damage, for both short and middle disease durations. In addition, after adjusting for confounding factors (age, sex, and SLEDAI-2K), no chronic damage accrual was associated with GC-free treatment status (overall response, 3.6; 95% confidence interval [CI], 1.1–11.3).
Conclusion
This study highlights that GC use can increase the risk of chronic damage in patients with SLE, with no chronic damage accrual independently related to a GC-free treatment status in patients with a disease duration of ≥20 years. In addition, patients with a longer disease duration were less likely to receive immunosuppressants and hydroxychloroquine, despite the use of both treatment potentially reducing the dose of GC required to avoid relapse. The lower use of hydroxychloroquine in this study compared with others may have been due to its 2016 approval in Japan. The authors highlighted several limitations of the study, including its cross-sectional nature, lack of cumulative dose data, and small subgroup sample sizes. Sada et al. concluded that due to the association of no damage accrual and GC-free treatment status, it is important to achieve a GC-free treatment status even in patients with longer disease durations.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

