All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Non-pharmacological management of patients with systemic lupus erythematosus: EULAR recommendations
Do you know... Which of the following statement relating to the overarching principles of the EULAR recommendations for non-pharmacological management of SLE is incorrect:
People living with systemic lupus erythematosus (SLE) continue to experience declining health-related quality of life (HRQoL) despite advancements in pharmacological treatment strategies over the past few decades.1,2 Growing evidence suggests that, alongside pharmacotherapy, the management of SLE should also integrate non-pharmacological interventions into routine care.1,2
While the use of non-pharmacological interventions, such as physical exercise and patient education, has increased in clinical practice, their implementation, content, delivery methods, and accessibility may be suboptimal or sometimes unsuitable. The lack of evidence-driven, standardized recommendations is a barrier to the widespread utility of non-pharmacological interventions.
The European Alliance of Associations for Rheumatology (EULAR) recently developed evidence-based recommendations on the non-pharmacological management of patients with SLE and systemic sclerosis (SSc). These recommendations were published by Parodis et al.1 in Annals of the Rheumatic Diseases, including a systematic review informing the recommendations, published in Rheumatic & Musculoskeletal Diseases Open.2 Here, we summarize the overarching principles and generic recommendations, as well as SLE-specific EULAR recommendations and the supporting evidence.
Methods1
A steering committee and taskforce were established, consisting of seven rheumatologists, 15 other healthcare professionals, and three patients. A systematic literature review was conducted to inform the EULAR recommendations. Overarching principles and recommendation statements were formulated by the steering committee, discussed with the task force through an iterative voting process, and graded based on level of evidence, level of agreement, and strength of recommendation.
Results1,2
Overarching principles and recommendations for non-pharmacological management of SLE1
Based on the evidence and expert opinion within the EULAR task force, four overarching principles were developed (Figure 1).
Figure 1. Overarching principles for non-pharmacological management of SLE*
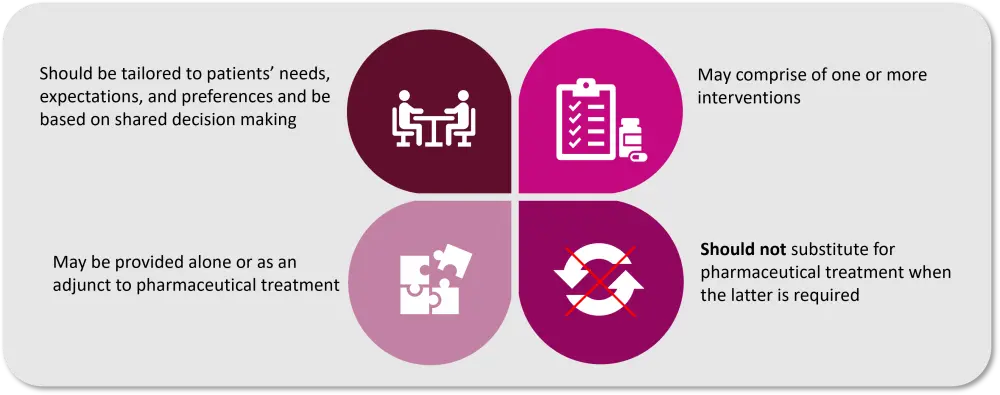
SLE, systemic lupus erythematosus.
*Adapted from Parodis, et al.1
Overall, 12 recommendations for the non-pharmacological management of patients with SLE and SSc were developed and categorized into three groups depending on the patient population: SLE and SSc, SLE, and SSc. Table 1 summarizes the recommendations for the non-pharmacological management of patients with SLE and SSc, and Figure 2 provides greater detail regarding the recommendations specifically for patients with SLE and strategies to implement them.
Table 1. Recommendations for the non-pharmacological management of patients with SLE and SSc*
|
SLE, systemic lupus erythematosus; SSc, systemic sclerosis. *Data from Parodis, et al.1 and Parodis, et al.2 |
|
Recommendation |
|---|
|
Non-pharmacological management should be directed toward improving health-related quality of life in people with SLE and SSc. |
|
People with SLE and SSc should be offered patient education and self-management support. |
|
In people with SLE and SSc, smoking habits should be assessed, and cessation strategies should be implemented. |
|
In people with SLE and SSc, avoidance of cold exposure should be considered for the prevention of Raynaud’s phenomenon. In people with SSc, this is of particular importance for the mitigation of severe Raynaud’s phenomenon. |
|
Physical exercise should be considered for people with SLE and SSc |
Figure 2. Recommendations for the non-pharmacological management of patients with SLE*
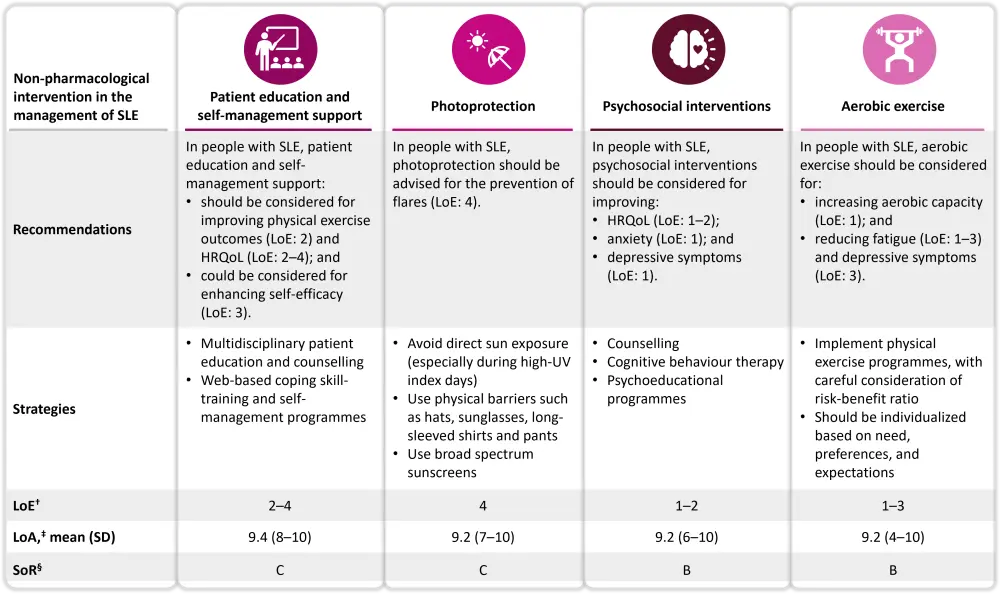
HRQoL, health-related quality of life; LoA, level of agreement; LoE, level of evidence; RCT, randomized controlled trial; SD, standard deviation; SLE, systemic lupus erythematosus; SoR, strength of recommendation; SSc, systemic sclerosis; UV, ultraviolet.*Data from Parodis, et al.1 and Parodis, et al.2
†LoE 1: Systematic reviews or meta-analyses of RCTs with consistent results; LoE 2: Well-conducted RCTs; LoE 3: Non-RCTs, cohort studies, case-control studies, or systematic reviews of these types of studies. LoE 4: Case series, case reports or studies with poor methodological quality; LoE 5: Expert opinion or consensus statements.
‡The level of agreement on a scale from 0 (complete disagreement) to 10 (complete agreement). §SoR ranged from A to D, with A comprising of consistent LoE 1 studies and D of LoE 4 or inconsistent studies.
*Data from Parodis, et al.1 and Parodis, et al.2
Summary of evidence informing EULAR recommendations
Patient education and self-management1,2
Evidence from a randomized controlled trial (RCT) showed that integrating patient education and self-management as part of physical exercise programs was effective in improving aerobic capacity and mental health in patients with SLE versus usual care. Another RCT found web-based patient education and counselling improved quality of life in patients with SLE. Other RCTs found that web-based patient education led to improvements in managing fatigue, sleep disturbances, and anxiety. Furthermore, a pilot RCT incorporating a web-based coping skill training program and a qualitative study of multidisciplinary patient education program showed improved HRQoL in patients with SLE.
Physical exercise1,2
A meta-analysis of six RCTs and five quasi-experimental studies revealed that exercise led to a significant improvement in aerobic capacity and a reduction in fatigue and depressive symptoms (Figure 3A). Moreover, physical exercise also improved physical functioning, as assessed by a meta-analysis of two RCTS measuring 36-Item Short Form Survey (SF-36).
Psychological interventions2
Two meta-analyses, including six RCTs, each found that psychological interventions were effective in managing anxiety, depressive symptoms, disease activity, stress, and SF-36 physical component summary scores (Figure 3B). Additionally, another meta-analysis of two RCTs found that cognitive behavioral therapy was associated with enhanced HRQoL in people with SLE.
Smoking cessation1
A meta-analysis of nine case-control studies revealed that the risk of developing SLE was around 50% higher in current smokers versus non-smokers (Figure 3C). Smoking also reduced treatment efficacy among patients with SLE. Another meta-analysis of 10 observational studies showed a negative association between smoking and the response of cutaneous SLE to antimalarial therapy. Also, several prospective cohort studies showed that, compared with non-smokers, smokers had reduced belimumab efficacy in SLE population.
Figure 3. Effect of A physical exercise, B psychosocial interventions, and C smoking cessation on SLE*
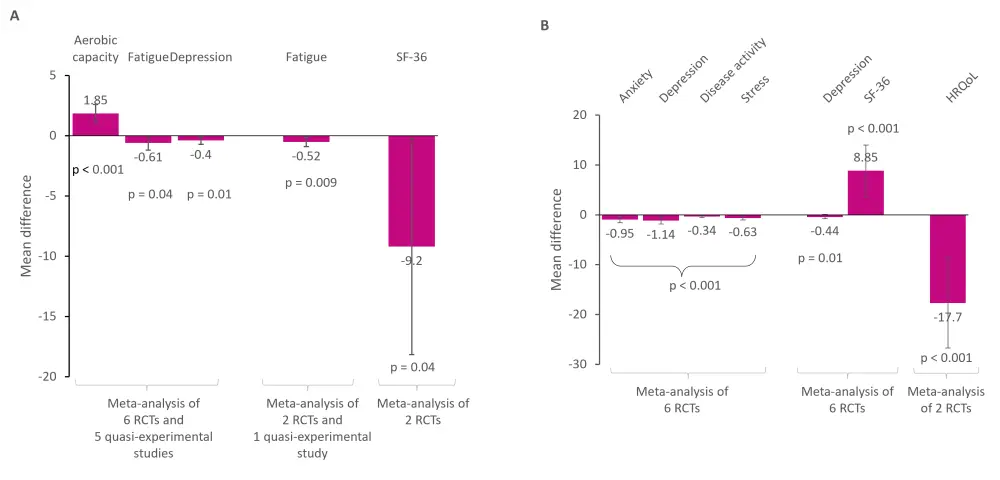
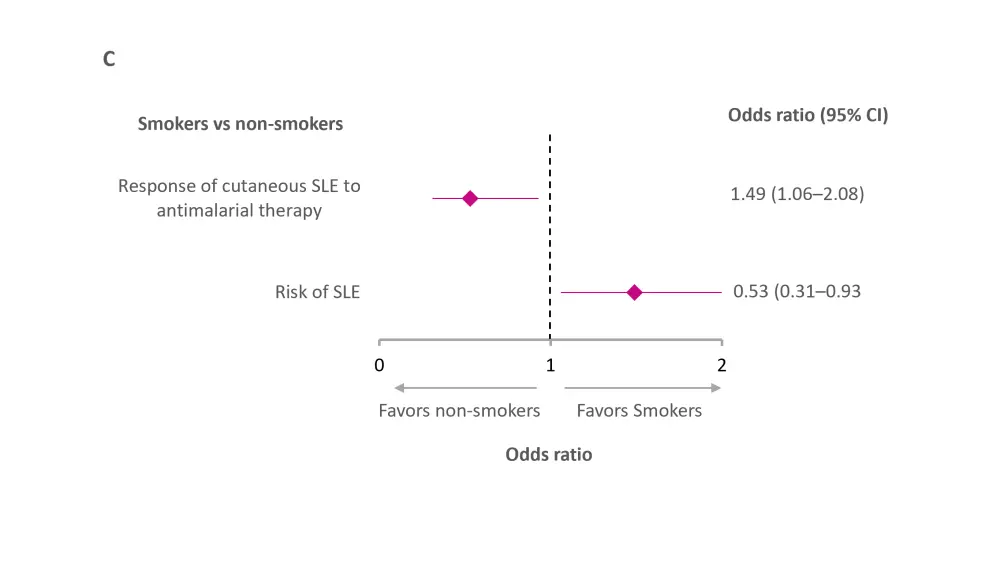
CI, confidence interval; HRQoL, health related quality of life; RCT, randomized clinical trial; SF-36, 36-Item Short Form Survey; SLE, systemic lupus erythematosus.
*Data from Parodis, et al.1 and Parodis, et al.2
Photoprotection1,2
Findings from quasi-experimental studies suggested that broad-spectrum sunscreens protected against upregulation of intracellular adhesion molecule-1 messenger ribonucleic acid expression and prevented photo-provocation-positive cutaneous lesions.
Other interventions2
There were a few additional findings from the systematic literature review, although these were not included in the EULAR recommendations. A few observational studies found increasing consumption of vitamin B6 and a vitamin C-rich diet to be linked with lower SLE disease activity. In addition, pulsed dye laser on discoid lesions was found to decrease mucocutaneous activity, as evaluated using the Cutaneous Lupus Erythematosus Disease Area and Severity Index in a quasi-experimental study.
Conclusion1,2
The EULAR recommendations for the use of non-pharmacological interventions in the management of SLE will guide healthcare professionals to provide holistic and personalized care for patients with SLE.
The level of evidence and strength of recommendations were limited by the heterogeneity of the studies; for instance, there was a lack of clear indication of blinding strategies used in the RCTs, a shorter follow-up period, limited exploration of dietary therapy, and limited evidence on wound management. The EULAR taskforce has formulated a research and educational agenda to address the need for higher evidence levels and increase awareness on how to assist patient education, improve clinician-patient communication, and facilitate shared-decision making. Further studies are warranted to identify the obstacles to integrating non-pharmacological management of SLE into routine care and to determine effective ways to mitigate these challenges.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

