All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Patient-reported outcomes in neuropsychiatric SLE: Post hoc analysis of four phase III trials of belimumab
Around 20% of patients with systemic lupus erythematosus (SLE) experience primary neuropsychiatric (NP) events, known as neuropsychiatric SLE (NPSLE). However, our understanding of the impact of NPSLE on patient-reported outcomes is limited.
Nikolopoulos, et al. recently published a post-hoc analysis of four phase III trials of belimumab in Rheumatology, in which they assessed the impact of neuropsychiatric involvement on patient-reported outcomes in patients with SLE.1 Here, we summarize their key findings.
Methods
-
Data from four phase III trials (BLISS-52 [NCT00424476], BLISS-76 [NCT00410384], BLISS-SC [NCT01484496], EMBRACE [NCT01632241]) were analyzed.
-
Patients with NP-British Isles Lupus Assessment Group (NP-BILAG) A/B/C/D or score in any descriptor of the NPSLE Disease Activity Index 2000 at baseline were categorized as having NPSLE.
-
-
Further, patients were subgrouped as having active NPSLE if scored A/B in the neuropsychiatric domain of BILAG and/or any neuropsychiatric descriptor scored in the SLE Disease Activity Index-2000.
-
Patients were subgrouped as having inactive NPSLE patients if had a BILAG score C/D in the neuropsychiatric domain and no neuropsychiatric descriptor scored in the SLE Disease Activity Index-2000.
-
-
Patients with NP-BILAG E were categorized within non-NPSLE.
-
Health-related quality of life (HRQoL) was assessed using three instruments:
-
-
Study Short Form 36 (SF-36);
-
Functional Assessment of Chronic Illness Therapy Fatigue (FACIT-F) scale, and
-
the three-level version of the EuroQol research foundation 5-dimension (EQ-5D-3L).
-
-
‘No problems’ in all EQ-5D dimensions indicated Full Health State (FHS).
-
Frequency of HRQoL outcomes were assessed in patients with active vs inactive NPSLE.
Key findings
-
A total of 2,968 patients were included in the analysis (non-NP SLE, n = 2,618; NPSLE, n = 350).
-
Mean age at baseline was 38.2 years and 94.6% of patients were female.
-
Patients with NPSLE vs non-NPSLE reported lower SF-36 physical component summary, SF-36 mental component summary, EQ visual analogue scale, and FACIT-F scores (Figure 1).
-
-
Significant differences were seen in all SF-36 subscales, namely physical functioning, role physical, bodily pain, general health, social functioning, vitality, role emotional, and mental health (p < 0.001).
-
-
The EQ-5D utility index scores were significantly worse in patients with NPSLE vs those with non-NPSLE (0.68 vs 0.75; p < 0.001).
-
-
The proportion of patients experiencing FHS was lower within the NPSLE group compared with the non-NPSLE group (3.3% vs 14.5%; p < 0.001).
-
A significantly lower proportion of patients with NPSLE reported no problems vs moderate or major problems in different dimensions of EQ-5D compared with the non-NPSLE group (Figure 2).
-
-
Patients with active NPSLE reported no significant differences in SF-36, FACIT-F, EQ visual analogue scale, EQ-5D utility index score, and EQ-5D FHS frequencies compared with those with prior but currently inactive NPSLE.
Figure 1. HRQoL between patients with NPSLE and non-NPSLE*
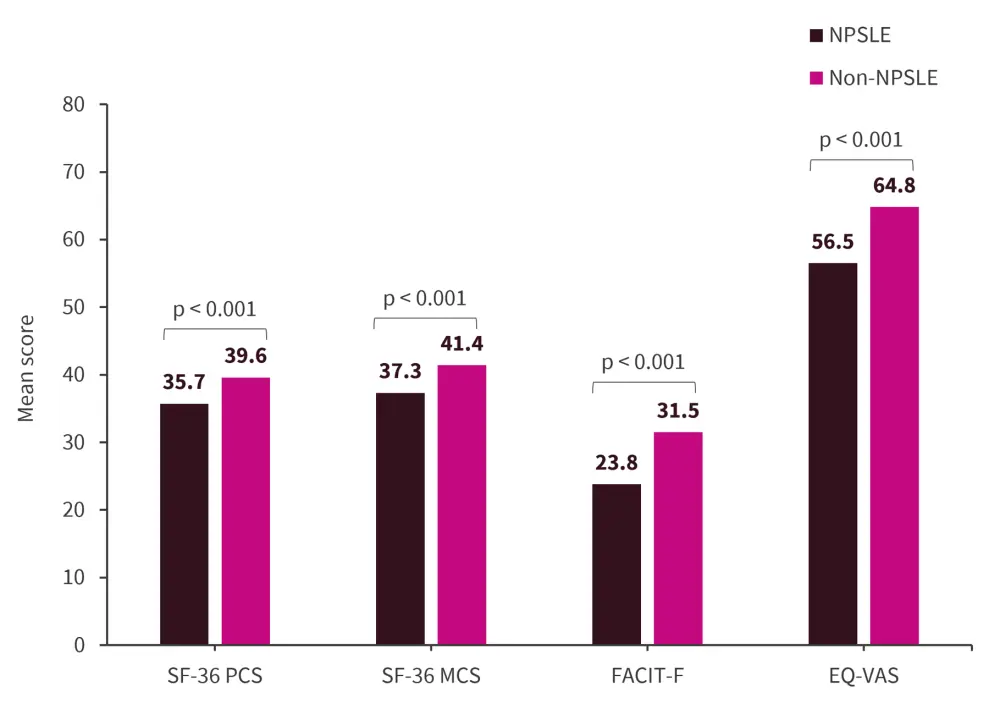
EQ-VAS, EuroQol visual analogue scale; FACIT-F, Functional Assessment of Chronic Illness Therapy – Fatigue; MCS, mental component summary; NPSLE, neuropsychiatric systemic lupus erythematosus; PCS, physical component summary; SF-36, Study Short Form 36.
*Adapted from Nikolopoulos, et al.1
Figure 2. Odds of having no problems vs moderate/major problems in different dimensions of EQ-5D in NPSLE vs non-NPSLE*
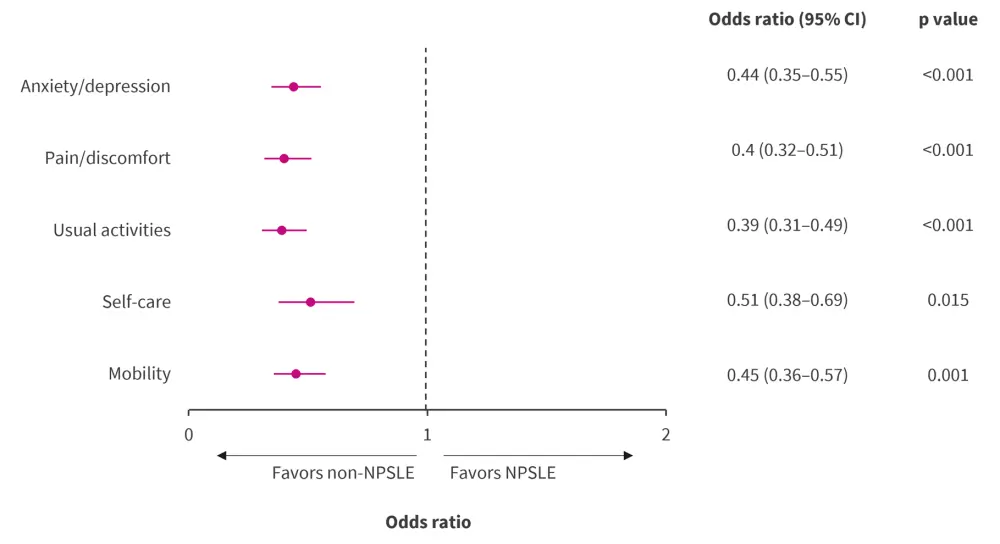
CI, confidence interval; EQ-5D, EuroQol research foundation 5-dimension; NPSLE, neuropsychiatric systemic lupus erythematosus.
*Data from Nikolopoulos, et al.1
|
Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

