All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Real-world long-term safety and efficacy of tacrolimus: Final analysis of the TRUST study
Lupus nephritis (LN) is a serious complication of systemic lupus erythematosus that contributes to increased morbidity and mortality. Tacrolimus, a calcineurin inhibitor, is approved in Japan and other Asian countries for the treatment of LN. However, there is a lack of robust data on its long-term safety and efficacy as a maintenance therapy in LN.
Here, we summarize an article published by Takeuchi et al. in The Journal of Rheumatology that assessed the 10-year safety and efficacy of tacrolimus as maintenance therapy in Japanese patients with LN treated in real-world clinical practice.1
Methods1
- TRUST was a 10-year, open-label, observational, non-comparative, post-marketing surveillance study (NCT01410747) conducted across 278 sites in Japan.
- Kaplan–Meier analysis was used to calculate tacrolimus continuation rate, cumulative incidence of adverse drug reactions (ADRs), relapse, and progression to renal failure and dialysis.
Key findings1
- A total of 1,355 and 1,353 patients were included in the safety and efficacy analysis sets, respectively.
- The mean age of patients was 38.3 years and 84.9% were women.
Treatment
- Over the 10-years of follow-up, the tacrolimus continuation rate was 49.3%. The most common reasons for treatment discontinuation were onset of adverse events (17.9%), unchanged/worsened symptoms (14.8%), symptoms improved (4.1%), and patient requests (4.8%).
- In the 94.6% of patients receiving corticosteroids at baseline, the mean prednisolone equivalent daily dose of oral corticosteroids reduced significantly from Week 4 (16 mg/day) to Year 10 (7.2 mg/day; p < 0.001).
Safety
- Over 10 years, 2,409 ADRs were reported in 60.6% of patients (Figure 1).
- The most commonly reported ADRs were hypertension (7.7%), nasopharyngitis (5.4%), herpes zoster and diarrhea (both 4.6%), upper respiratory tract inflammation (4.1%), bronchitis (3.8%), increased blood creatinine (3.7%), hyperuricemia (3.2%), diabetes mellitus (3.1%), pharyngitis (3.0%), gastroenteritis and renal impairment (both 2.9%), cystitis (2.4%), constipation (2.3%), and pneumonia (2.1%).
- The most frequently reported serious ADRs were infections (Figure 1).
- There was no marked increase in incidence of any ADR or serious ADR over time.
- Overall, 48 patients (3.5%) died over the 10 years of follow-up.
Figure 1. Incidence of ADRs and serious ADRs over 10 years of follow-up*
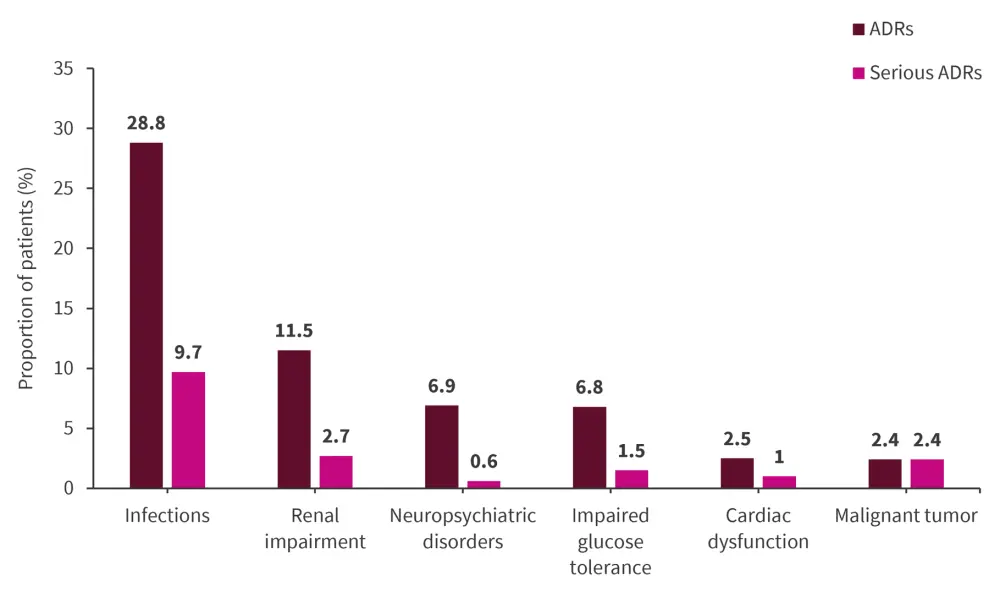
ADR, adverse drug reaction.
*Data from Takeuchi, et al.1
Efficacy
- In the efficacy analysis set (n = 1,353), the cumulative rate of relapse was 44.5% at 10 years.
- In the renal prognosis analysis set (n = 1,140), the cumulative rates of progression to renal failure and dialysis were 12.2% and 4.5%, respectively, at 10 years.
- Serum creatinine levels were relatively consistent from Year 1 through Year 10.
- The estimated glomerular filtration rate at baseline (80.9 mL/min/1.73 m2) decreased significantly from Week 4 (79.3 mL/min/1.73 m2) to Year 10 (68.3 mL/min/1.73 m2; p < 0.001).
|
Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

