All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Systematic review and meta-analysis of mental health conditions in patients with SLE
Mental health conditions (MHCs) are prevalent among patients with systemic lupus erythematosus (SLE) across age groups. However, it remains unclear whether MHCs are associated with an increased risk of SLE or influence the subsequent outcomes of the disease.
Liu X et al.1 recently published an article in Rheumatology (Oxford) sharing a systematic review and meta-analysis to estimate the pooled prevalence of MHCs in patients with SLE and their association with risk and outcomes of the disease. Here, we summarize their key findings.
Methods1
- Studies published before 2023 were searched in PubMed, Web of Science, and EMBASE.
- Prevalence of MHCs were pooled separately for two age groups (adults aged ≥18 years vs children aged <18 years) and then according to outcome measures within each category.
- Using random-effect models, pooled prevalence and risk ratios were calculated for each MHC.
Key findings1
- Of 203 identified studies (N = 1,485,094), 189 studies (12 studies among children and 177 in adults) evaluated the prevalence of MHCs in patients with SLE.
Prevalence of MHCs among patients with SLE
- Among adults with SLE, the most prevalent mental disorders were cognitive impairment, mood disorder, and depressive disorder, while the most prevalent mental health symptoms were sleep disturbance, anxiety symptoms, and cognitive dysfunction (Figure 1A).
- Among children with SLE, the most prevalent mental disorder and mental health symptom was cognitive impairment and dysfunction, respectively (Figure 1B).
Figure 1. Prevalence of mental health conditions among A adults and B children with SLE*
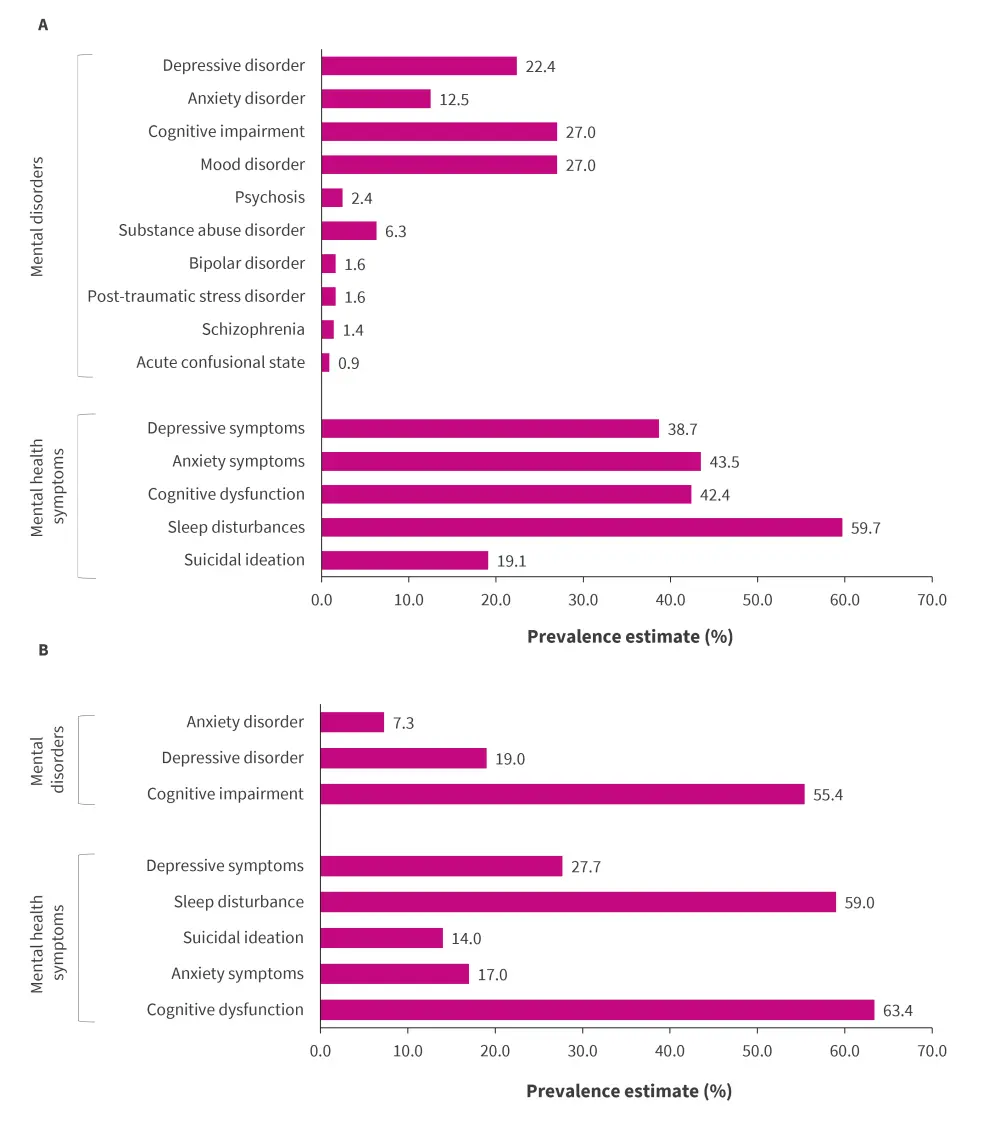
SLE, systemic lupus erythematosus.
*Data from Liu X, et al.1
Association between pre-existing MHCs and the risk of SLE
- Eight cohort studies (N = 1,316,921 adults) reported association of MHCs prior to SLE diagnosis and the risk of SLE.
- Five studies reported that post-traumatic stress disorder was associated with a higher risk of SLE (risk ratio = 1.93; p < 0.001).
- Two studies demonstrated that depressive disorder was associated with an increased incidence of SLE (risk ratio = 2.30; p < 0.001).
- One study showed association between all types of sleep disorders and increased risks of SLE.
MHCs and patient outcomes of SLE
- Seven studies reported associations between MHCs and clinical outcomes in patients with SLE.
- Depressive symptoms were associated with adverse outcomes, including a higher risk of unemployment and subclinical atherosclerosis, and decreased health-related quality of life.
- Anxiety showed no significant association with progression of SLE disease activity.
- Clinically diagnosed mental disorders were found to increase intensive care unit admissions over time and suicidal drug overdoses.
| Key learnings1 |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

