All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
An overview of risk factors and strategies for managing pregnancy in women with systemic lupus erythematosus
Do you know... What is the relative frequency of preterm birth in pregnancies of women with SLE compared with those in the general population?
The occurrence of systemic lupus erythematosus (SLE) is notably higher among women in their reproductive years. Despite advancements in the management of pregnancies among women with SLE, a higher risk of adverse maternal and fetal outcomes persists compared to the general population.1 The Lupus Hub has previously presented a retrospective cohort study on SLE disease activity at conception, during pregnancy, and after birth.
In the below article, we summarize the recently published reviews on pregnancy in SLE by Zuchhi et al.1 and Sangah et al.2 in Best Practice & Research Clinical Rheumatology and Journal of Obstetrics and Gynaecology, respectively, and drug compatibility in pregnant women with SLE as per American College of Rheumatology (ACR) guidelines, published by Sammaritano et al. in Arthritis Care & Research (Hoboken). We aim to provide an overview of the potential impact of pregnancy on SLE and vice versa, risk factors for adverse maternal and fetal outcomes, importance of preconception counseling, and drug compatibility during pregnancy in women with SLE.
Impact of pregnancy on SLE
Disease flares1
SLE typically follows a relapsing-remitting course, with flares manifesting at any point during pregnancy and postpartum; rates range between 25% and 70%. The most frequent manifestations include arthritis, hematologic, and skin-related symptoms.1 The major risk factors for flares in pregnancy are shown in Figure 1.
Figure 1. Risk factors for SLE flares and pregnancy complications*
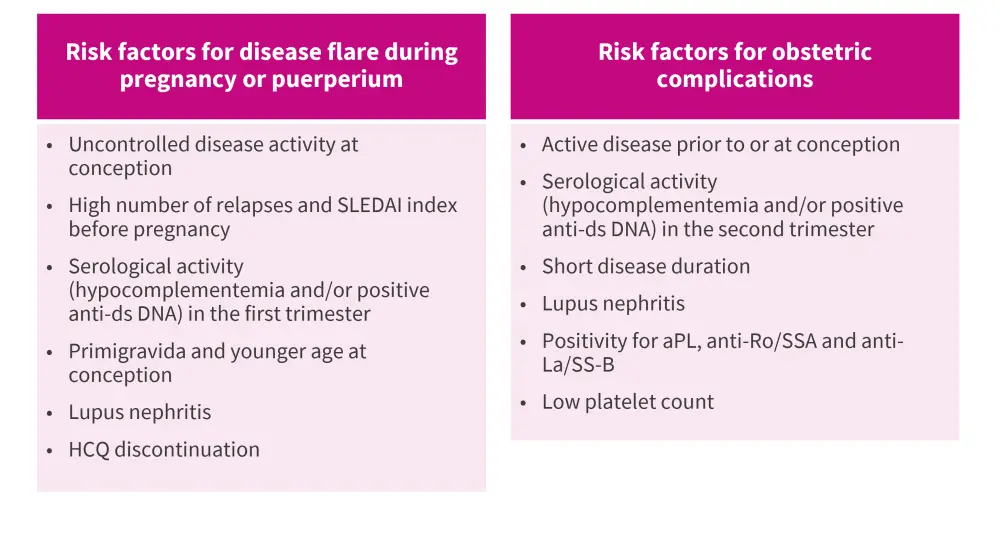
aPL, antiphospholipid antibodies; DNA, deoxyribonucleic acid; dsDNA, double stranded DNA; HCQ, hydroxychloroquine; SLE, systemic lupus erythematosus; SLEDAI, SLE Disease Activity Index.
*Adapted from Zucchi, et al.1
Lupus nephritis1
During pregnancy or the postpartum period, diagnosis of new lupus nephritis (LN) was reported in 4–30% of women with SLE. While women with previous history of LN carry a 20–30% risk of experiencing relapse during their pregnancy.1
Impact of SLE on pregnancy1,2
Infertility2
Evidence from existing literature highlights the difficulties in conception among women with SLE. Furthermore, there is an increased likelihood of miscarriage and pregnancy-related disorders influenced by immunological factors, such as presence of anticardiolipin antibodies.
Maternal outcomes1,2
Preeclampsia1,2
Preeclampsia affects up to 30% of SLE pregnancies compared to 3.4% of all pregnancies in the United States.2 Risk factors of preeclampsia in women with SLE include renal involvement, thrombocytopenia, and antiphospholipid antibodies (aPL) positivity.1
Emerging evidence suggests that natural killer cells (NKCs) play a pivotal role in maintaining a pro-inflammatory microenvironment in the decidua of healthy pregnancies. Inadequate activation of NKCs leads to poor decidual artery remodeling and increases the risk of preeclampsia. Hence, presence of NKCs and endothelial progenitor cells in the blood may serve as biomarkers for early diagnosis of preeclampsia.2
Hypothyroidism2
Thyroid disease is more prevalent in pregnant women with SLE compared with those in the general population. In addition, hypothyroidism and auto-immune thyroid disease, characterized by the presence of thyroid antibodies with or without thyroid dysfunction, are common in women with SLE.
Neurological symptoms2
SLE can affect the central nervous system with manifestations ranging from headache and cognitive impairment to life-threatening conditions, such as memory loss, seizures, and stroke. While stroke and transient ischaemic attacks are less common in SLE, the presence of aPL antibodies is believed to be a contributing factor to arterial and venous thrombosis.
Infection2
Given that pregnancy itself is associated with a weaker immune state, SLE substantially increases the risk of infection in pregnant women; SLE is caused by immune system dysregulation and excessive autoantibody production.
Fetal mortality1,2
Pregnancy loss is one of the most prevalent maternal complications, observed in around 16.5% women with SLE.1,2 The risk factors for pregnancy loss in SLE include active disease and low complement or positive anti-double stranded DNA in the second trimester.1
Fetal outcomes1,2
Preterm birth1,2
Preterm birth is one of the most common obstetric complications, affecting about 30–40% women with SLE, compared with 12% in the general population.1
The major risk factors for preterm birth in pregnant women with SLE include activation of the maternal or fetal hypothalamus-pituitary axis, local and systemic inflammation from infections, autoantibodies, lower estrogen levels, and treatment with oral prednisone.2 Preterm births are more commonly observed in women with disease activity at conception due to increased inflammation and autoantibodies, immunological alterations, and medications used.2 In addition, SLE patients have higher rates of cesarean delivery compared to other women.1
IUGR and SGA neonate1
Studies have reported a higher incidence rate of intrauterine growth restriction (IUGR) in women with SLE than in the general population (5.3% vs 1.6%). The incidence is highest during active disease at conception or 6 months preceding pregnancy.1 One of the major risk factors for IUGR in SLE pregnancies is the presence of aPL.
Also, the incidence rate of small for gestational age infants has been reported to be significantly higher in SLE pregnancies compared to those in general population (25% vs 4.5%). However, in recent years, the IUGR and small for gestational age rates have declined to 2.6% and 12.2%, respectively, reflecting improvements in SLE management during pregnancy.
Neonatal lupus syndrome1,2
Neonatal lupus occurs due to the transplacental passage of autoantibodies, anti-Ro/SSA and anti-La/SS-B, from mother to child, usually during second trimester of gestation.1,2
The most common manifestation of cardiac neonatal lupus is congenital heart block which needs pacing for survival.1,2 In cases of mothers with anti-Ro/SS-A and with previous child with congenital heart block, the risk increases to up to 18%.1,2 The key risk factors for obstetric complications in SLE pregnancies are listed in Figure 1.
Pre-conception counseling1
Pre-conceptional counseling with the patient and her partner is required to prevent unplanned pregnancies, stratify the single-patient pregnancy risk, and minimize adverse pregnancy outcomes through proper education and appropriate treatment. The key objectives of a pre-conception visit are outlined in Figure 2.
Figure 2. Goals of pre-conception counselling*

*Adapted from Zucchi, et al.1
Treatment1
Treatment approaches should be tailored based on each individual patient's disease activity, response to medications, and potential pregnancy complications. Medications, such as hydroxychloroquine, azathioprine, low-dose glucocorticoids, and low-dose aspirin with or without low-molecular-weight heparin are considered safe during SLE pregnancies; while cyclophosphamide, methotrexate, and mycophenolate are contraindicated. Of note, continuation of hydroxychloroquine during SLE pregnancies has proven its role in controlling disease activity, and reducing risk of pre-eclampsia, IUGR, and pre-term birth. Hence, it should not be discontinued during pregnancy as it could potentially trigger a disease flare.1
The drug compatibility during pregnancy and lactation, as per the 2020 ACR guidelines, is detailed in Figure 3.1,3
Figure 3. Drug compatibility during pre-conception, pregnancy, and lactation*
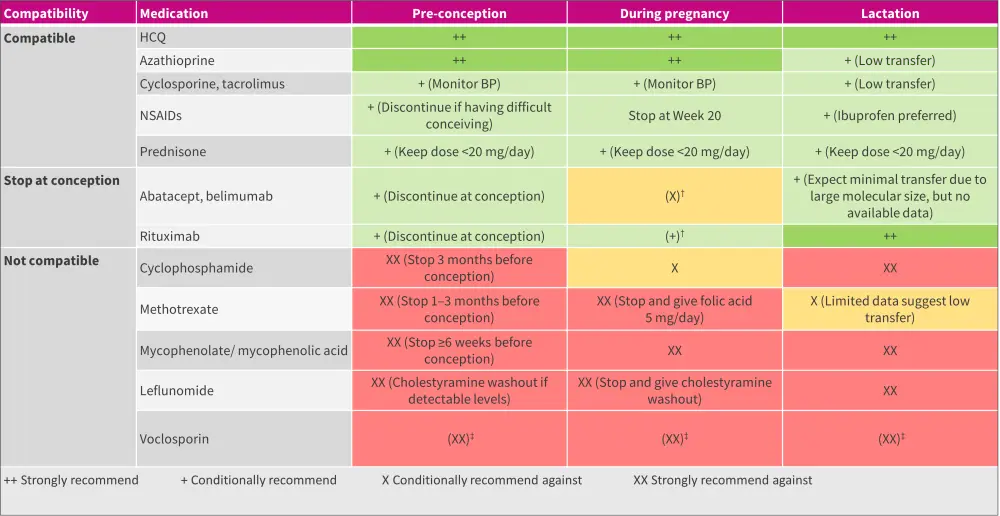
BP, blood pressure; HCQ, hydroxychloroquine; NSAID, non-steroidal anti-inflammatory drug.
*Adapted from Zucchi, et al.1 and Sammaritano, et al.3
†Continuation during pregnancy should be decided on an individual basis.
‡Due to the alcohol content in the formulation.
Conclusion1,2
Pregnant women with SLE are at a higher risk of adverse maternal and fetal outcomes compared with the general population. Various risk factors have been identified, such as uncontrolled disease activity at conception, concomitant APS or aPL positivity, LN, etc. Improving pregnancy outcomes in women with SLE requires thorough pre-conception counseling, close clinical monitoring, and potential medication adjustments.
Further studies are required to assess additional markers capable of identifying women at higher risk of pregnancy complications. Additionally, the potential utilization of novel drugs in the management of SLE pregnancies needs to be investigated.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


