All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Identifying unmet needs in European patients with lupus nephritis
Do you know... What is the proportion of patients with SLE progressing to LN within 5 years of SLE diagnosis?
Lupus nephritis (LN) is a common and serious complication of systemic lupus erythematosus (SLE), associated with substantial morbidity and increased risk of end-stage renal disease (ESRD). Despite current standard of care (SOC), many patients fail to achieve sustained remission, resulting in adverse disease outcomes.1
At the 60th European Renal Association (ERA) Congress, Barratt et al.1 presented a targeted literature review (TLR) summarizing evidence on the burden of comorbidities, long-term renal outcomes, and real-world effectiveness of existing treatments in European patients with LN.1 Below, we summarize the key highlights.
Methods1
A TLR was performed using separate search strategies for various databases to identify relevant peer-reviewed articles in English, published between March 2012 and March 2022. Conference abstracts indexed in Embase from 2019 were also included. The records were screened by a single reviewer based on pre-defined inclusion and exclusion criteria.
Results1,2
A total of 4,216 records were identified, of which 55 studies were included in the final review (Figure 1). Most of the studies were observational and retrospective in design.
Figure 1. PRISMA diagram*
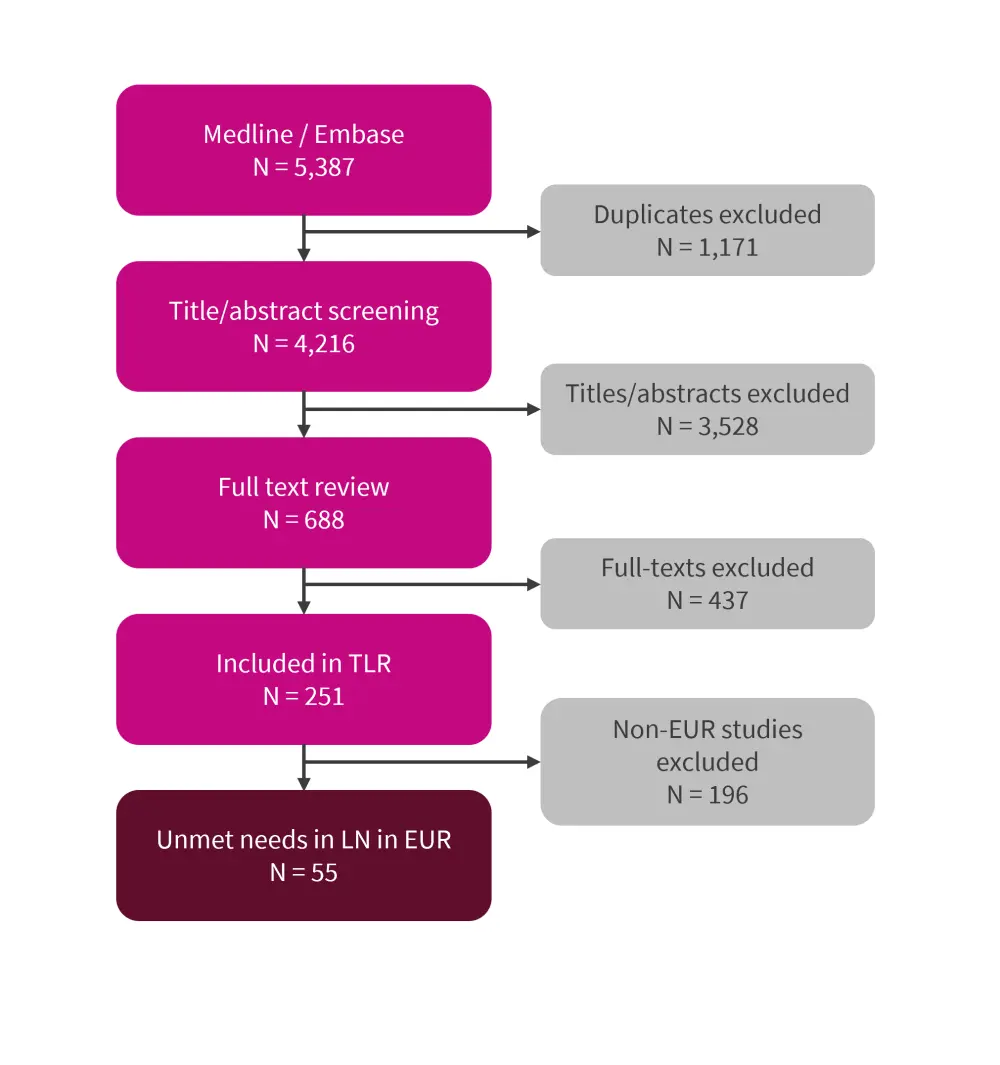
EUR, Europe; LN, lupus nephritis; PRISMA, preferred reporting items for systematic reviews and meta-analyses; TLR, targeted literature review.
*Data from Barratt.1
Comorbidities and mortality1,2
Among patients with SLE, up to 36% progressed to LN, with the majority of LN cases occurring within 5 years of SLE diagnosis.2
Adults with LN often suffered from comorbidities such as serious infection (19–35%), cardiovascular disease (CVD, 26%), and chronic kidney disease (CKD) or ESRD (6–22%). Patients developing LN were more likely to experience cardio- and cerebrovascular events than patients with SLE only (p = 0.001).2
The risk of mortality was significantly higher among patients with LN compared to those with SLE only or other lupus manifestations (p < 0.001). The most common causes of death were infections (8–32%), CVD (22–58%), or malignancies (5–27%). ESRD appeared to be an independent risk factor for mortality among these patients. Patients with LN and ESRD had a three-times higher mortality risk compared with those who had LN only (p < 0.001; Figure 2).1
Figure 2. Odds of mortality among patients with LN and ESRD compared with patients with LN only*
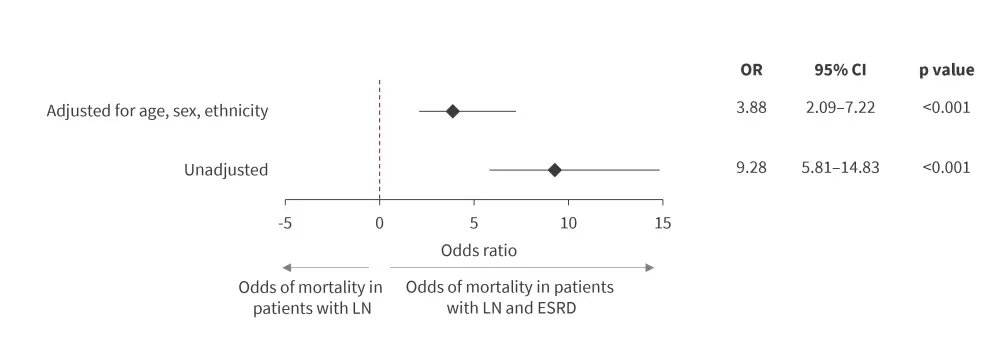
CI, confidence interval; ESRD, end-stage renal disease; LN, lupus nephritis; OR, odds ratio.
*Data from Barratt.1
Treatment response and relapses1,2
The majority of real-world studies utilized cyclophosphamide and mycophenolate mofetil as SOC therapy. Response rates varied across the studies, possibly due to heterogeneity in study design, patient population, drug dosing, etc. Comparative studies did not identify significant differences in response rates between the treatment regimens.2
Within the first year of starting SOC therapy, around 30–86% of patients with LN achieved complete renal response/remission (CRR). However, only 38% of patients were able to maintain CRR over 5-years and only 16% were able to maintain CRR over the 15-year follow-up period.1
Rituximab treatment resulted in 29–64% of patients with refractory LN achieving CRR after 12 months, while belimumab treatment resulted in 35% of patients with active LN despite SOC achieving CRR after 12 months.1
Over 3–6 years of follow-up, 20–35% of patients experienced a renal relapse/flare while on maintenance therapy, despite showing an initial response to current SOC.1
Impact of treatment response on renal outcomes1
After 1 year of treatment, non-responders had a significantly increased risk of mortality and CKD compared with responders (p < 0.004).
At 15 years, patients achieving a CRR had significantly longer CKD-free survival compared with non-responders (Figure 2).
Figure 3. Rate of renal relapse or flare after remission*
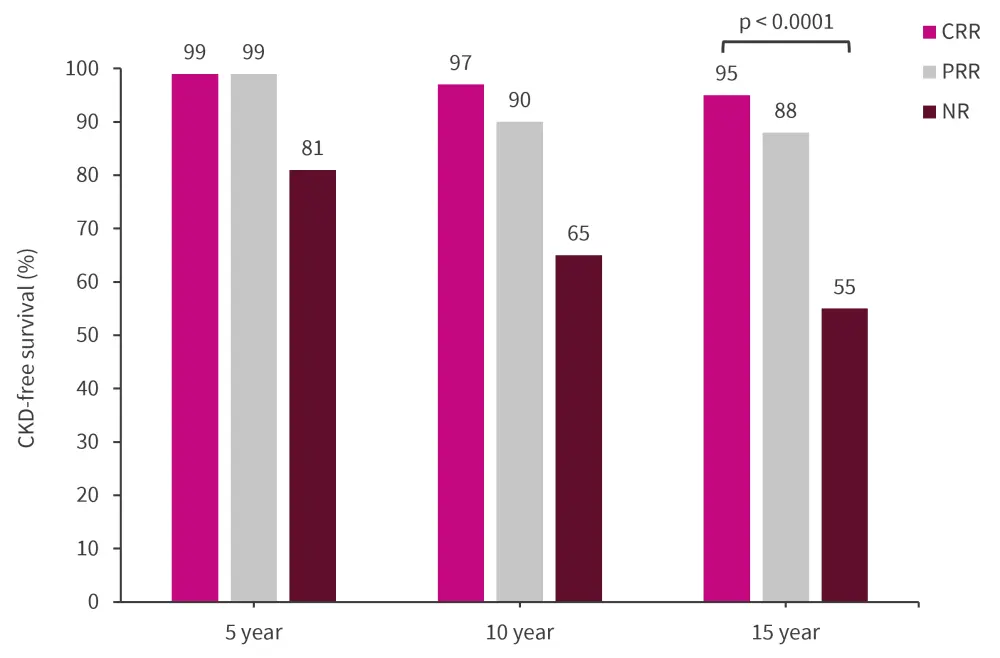
CRR, complete remission/response; NR, no response; PRR, partial remission/response.
*Adapted from Barratt.1
Conclusion1
Findings from this TLR highlighted the considerable comorbidity burden and poor long-term renal outcomes in patients with LN. CRR was achieved and maintained in few patients, and a notable proportion of patients who initially responded to therapy went on to encounter renal relapse. Given the potential benefits of achieving CRR in mitigating the risk of long-term renal complications, there is a clear need for effective therapies which can provide sustained remission, particularly for patients with severe/refractory LN.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

