All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Physician global assessment for type 2 manifestations of systemic lupus erythematosus
Systemic lupus erythematosus (SLE) manifestations are categorized as type 1 (classic signs and inflammatory symptoms) and type 2 (including symptoms of fatigue, depression, widespread pain, and brain fog). The type 2 manifestations, substantially impacting the quality of life, are reported more frequently by people living with SLE.
The existing physician/provider global assessments (PGAs) for measuring SLE activity do not encompass type 2 manifestations. To address this gap, Clowse et al.1 developed and psychometrically evaluated a novel PGA for type 2 symptoms (Type 2 PGA). Here, we summarize their key findings published in Lupus Science and Medicine.
Methods
Six rheumatologists at the Duke Lupus Clinic participated in a roundtable discussion to establish consensus guidelines for scoring the Type 2 PGA. Subsequently, psychometric evaluation was conducted using prospective data from patients with SLE enrolled in the Duke Lupus Registry since 2018.
At each visit, the treating rheumatologists completed the disease activity measures, including SLE Disease Activity Index (SLEDAI), and Type 1 and 2 PGAs, while patients completed the following questionnaires:
- Polysymptomatic Distress Scale (PSD), consisting of two subscales: the Widespread Pain Index (WPI) and the Symptom Severity Score (SSS); and
- Systemic Lupus Activity Questionnaire (SLAQ).
Key findings
Development
In total, 30 cases of patients with SLE were reviewed, with a median patient age of 37.5 years and with 57% having a history of nephritis. The Type 2 PGA scale and the proposed guideposts for scoring Type 2 PGA are depicted in Figure 1.
Figure 1. Guideposts for scoring Type 2 physician global assessment in SLE*
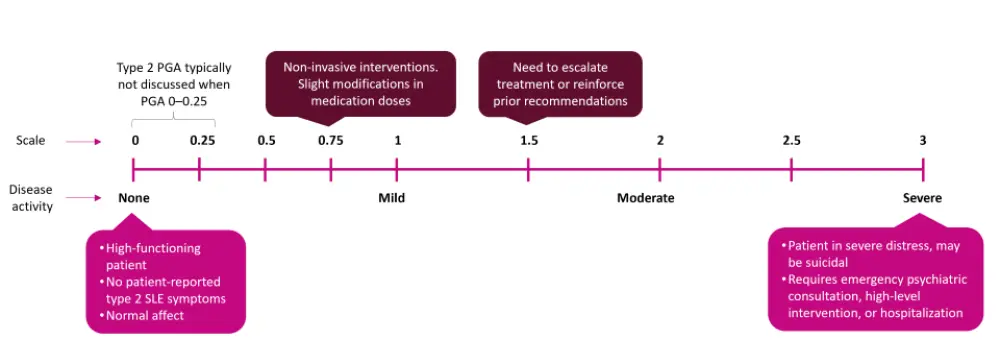
PGA, physician/provider global assessment; SLE, systemic lupus erythematosus.
*Adapted from Clowse, et al.1
Psychometric evaluation
A total of 263 patients were evaluated. The median age was 44 years, and 92% were female.
- Construct validity: The Type 2 PGA showed strong correlation with the total PSD and SSS, and moderate correlation with individual components of the PSD and SLAQ. Its weak correlation with type 1 PGA indicates that it evaluated a distinct construct (Figure 2).
- Known groups validity: The mean Type 2 PGA score increased with each severity category of PSD, with non-overlapping 95% confidence intervals.
- Test-retest reliability: Among 72 patients with consistent PSD score between two visits, the Type 2 PGA score at each visit had an intraclass correlation coefficient (ICC) of 0.69, indicating moderate reliability.
- Responsiveness to change: Among 152 patients with two visits, change in Type 2 PGA scores showed weak correlation with change in PSD scores between visits (r = 0.28; p < 0.001).
- Intra- and inter-rater reliability: Among 50 cases, the ICC between two scores was 0.83, showing good consistency of the score by a single rheumatologist and across multiple rheumatologists.
Figure 2. Construct validity of Type 2 PGA: Correlations of Type 2 PGA with patient-reported measures and type 1 SLE activity measures*
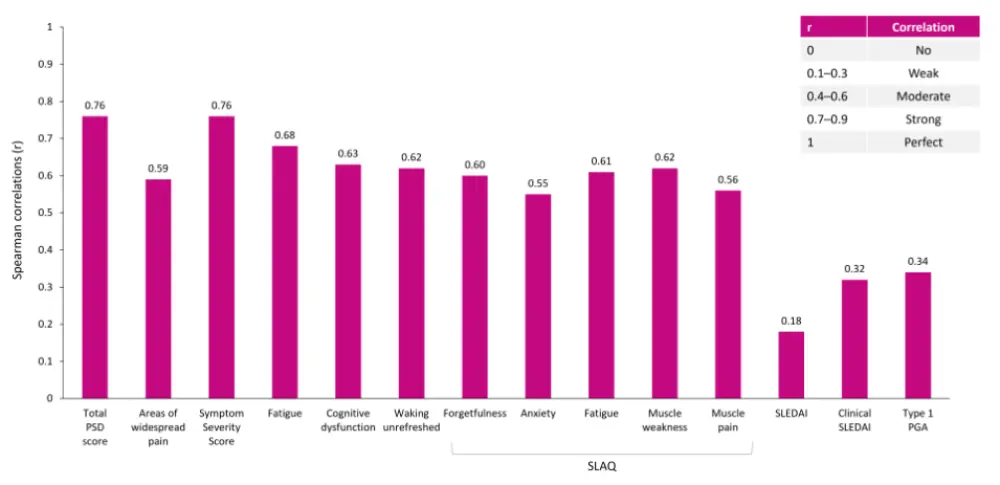
All p < 0.001.
PGA, physician/provider global assessment; PSD, Polysymptomatic Distress Scale; SLAQ, Systemic Lupus Activity Questionnaire; SLE, systemic lupus erythematosus; SLEDAI, SLE Disease Activity Index.
*Data from Clowse, et al.1
| Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content



