All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Using the EULAR/ACR criteria to assess organ damage in patients with SLE and LN
Long-term organ damage is a concern for patients with systemic lupus erythematosus (SLE), both through progression of the disease itself and the impact of treatments, such as the use of glucocorticoids.1 Assessing the degree of organ damage is vital for the appropriate management of these patients. In addition, determining which factors can lead to an elevated risk of organ damage, and therefore require more rigorous treatment, is key.2
To investigate this, we summarize two recent articles below. The first, by Mok et al.,3 investigated the relationship between European League Against Rheumatism (EULAR)/American College of Rheumatology (ACR) criteria and organ damage. The second, by Munhoz et al.,4 evaluated the impact of lupus nephritis (LN) on the short-term accrual of EULAR/ACR domains.
Association between EULAR/ACR criteria and organ damage3
Study design
From a previous cohort of patients with SLE (N = 542), validated using the 2019 EULAR/ACR criteria, patients were split into two groups according to EULAR/ACR score with a threshold of 20 used to define high and low scores.
Organ damage was assessed using the Systemic Lupus International Collaborating Clinics (SLICC)/ACR Damage Index (SDI). This tool includes 41 items to measure irreversible organ damage (not caused by active inflammation) across 12 organ systems.
Results
The mean age of patients was 36.2 years and 93.7% were female. EULAR/ACR features that were significantly increased in patients with a score ≥20 compared with scores of 10–19 are shown in Table 1; these included acute cutaneous lupus, pleural/pericardial effusion, leukopenia, and all renal and complement categories.
Table 1. Selected baseline patient characteristics and significant EULAR/ACR features*
|
ACR, American College of Rheumatology; ds, double stranded; EULAR, European League Against Rheumatism; SD, standard deviation; Sm, smith. |
|||
|
Characteristic, % (unless stated otherwise) |
Score 10–19 |
Score ≥20 |
p value |
|---|---|---|---|
|
Age at diagnosis (SD), years |
42.0 (±12.9) |
34.0 (±13.7) |
0.46 |
|
Female |
94.7 |
93.4 |
0.58 |
|
Follow-up duration (SD), years |
9.7 (±6.4) |
12.0 (±6.5) |
0.48 |
|
Features in EULAR/ACR criteria |
|||
|
Fever† |
4 |
13.5 |
0.001 |
|
Alopecia |
12.7 |
22.4 |
0.01 |
|
Oral ulcers |
5.3 |
16.1 |
0.001 |
|
Acute cutaneous lupus |
14.7 |
47.2 |
<0.001 |
|
Joint involvement |
54.7 |
70.4 |
0.001 |
|
Pleural/pericardial effusion |
4.7 |
17.3 |
<0.001 |
|
Seizure |
0 |
4.1 |
0.01 |
|
Leukopenia |
69.3 |
82.1 |
<0.001 |
|
Autoimmune hemolysis |
12.0 |
22.4 |
0.006 |
|
Proteinuria >0.5 g |
16.7 |
66.6 |
<0.001 |
|
Class II/V lupus nephritis by biopsy |
4.7 |
29.7 |
<0.001 |
|
Class III/V lupus nephritis by biopsy |
7.3 |
41.3 |
<0.001 |
|
Anti dsDNA antibody |
66.7 |
91.6 |
<0.001 |
|
Anti-Sm antibody |
14.7 |
27.6 |
0.002 |
|
Anti-phospholipid antibodies (lupus anticoagulant, anti-cardiolipin, or anti-β2-glycoprotein-1 antibody) |
16.7 |
28.1 |
0.006 |
|
Low C3 or C4 |
76.0 |
96.4 |
<0.001 |
|
Low C3 and C4 |
49.3 |
88.5 |
<0.001 |
Overall, 42.8% of patients had an SDI score ≥1, indicating organ damage at their last clinic visit. The SDI scores for both groups are shown in Figure 1, with the significantly different categories indicated. The total SDI score for patients with scores 10–19 was 0.67 (standard deviation [SD], ±1.03), this was significantly lower than 0.90 (SD, ±1.26) recorded for the ≥20 score group (p = 0.04).
Figure 1. Organ damage assessed by SDI between the two groups of EULAR/ACR criteria scores*
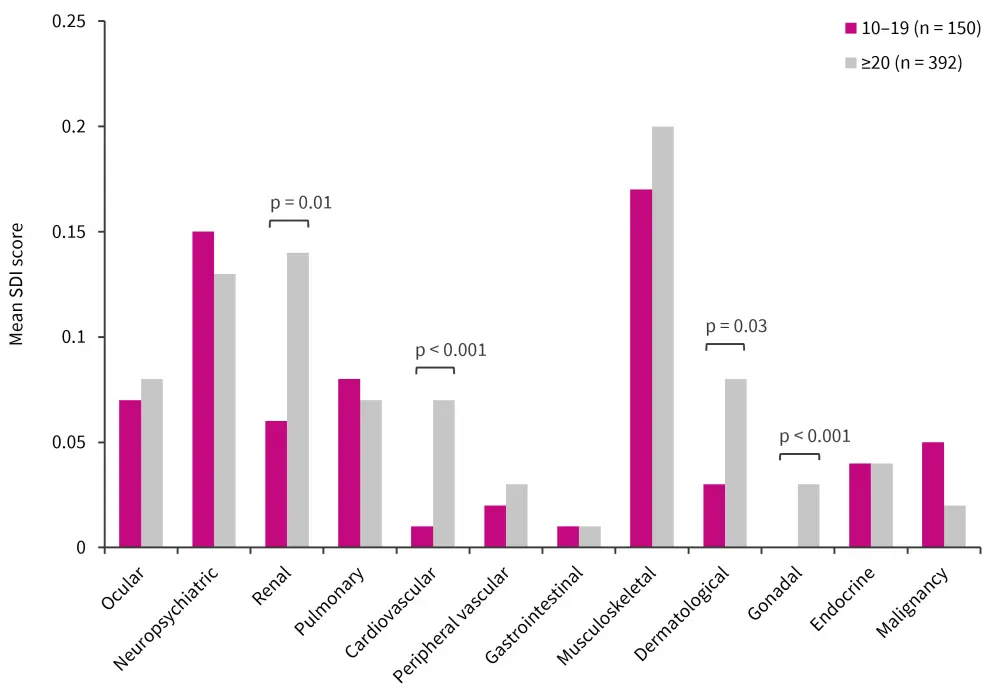
ACR, American College of Rheumatology; EULAR, European League Against Rheumatism; SDI, Systemic Lupus International Collaborating Clinics/ACR Damage Index.
*Adapted from Mok, et al.3
The EULAR/ACR criteria score uses seven clinical and three immunological domains together with an ANA (titer ≥1:80) to create a weighted score. If a patient scores ≥10 points when at least one clinical criterion is fulfilled, they are classified as having SLE.5
The correlation between SDI score and domains of the EULAR/ACR criteria was assessed and found to be weak overall. However, a positive correlation, after adjusting for age, sex, and follow-up duration, was found between EULAR/ACR criteria and the following domains3:
- renal (Rho, 0.11; p = 0.02)
- antiphospholipid antibodies (Rho, 0.11; p = 0.001)
- neuropsychiatric (Rho, 0.06; p = 0.02)
Total SDI score was also found to be positively correlated with EULAR/ACR criteria score after being adjusted for the same factors (Rho, 0.07; p = 0.01).
Further analysis was performed to assess correlations between EULAR/ACR domains and the domains of the SDI; categories that were significantly correlated are shown in Table 2. The strongest correlation was between the renal EULAR/ACR domain and the renal SDI domain.
Table 2. Significant correlations between EULAR/ACR criteria and SDI*
|
AB, antibody; ACR, American College of Rheumatology; EULAR, European League Against Rheumatism; SLE, systemic lupus erythematosus. |
||||
|
EULAR/ACR criteria domain |
SDI domain |
Rho |
p value |
Adjusted p value† |
|---|---|---|---|---|
|
Renal |
Renal |
0.30 |
<0.001 |
<0.001 |
|
Neuropsychiatric |
Neuropsychiatric |
0.17 |
<0.001 |
<0.001 |
|
Mucocutaneous |
Dermatological |
0.19 |
<0.001 |
<0.001 |
|
Renal |
Gonadal |
0.12 |
0.005 |
0.07 |
|
Neuropsychiatric |
Gonadal |
0.12 |
0.009 |
0.008 |
|
Musculoskeletal |
Gonadal |
0.09 |
0.04 |
0.14 |
|
Hematological |
Musculoskeletal |
0.09 |
0.04 |
0.08 |
|
Anti-phospholipid ABs |
Peripheral vascular |
0.18 |
<0.001 |
<0.001 |
|
Anti-phospholipid ABs |
Gastrointestinal |
0.13 |
<0.001 |
0.005 |
|
Anti-phospholipid ABs |
Neuropsychiatric |
0.13 |
0.003 |
<0.001 |
Following correlation analysis, patients with renal involvement were examined further. Patients with LN were significantly more likely to show damage in ophthalmologic, renal, cardiovascular, and gonadal domains of the SDI compared with patients without renal involvement.
Patients with a EULAR/ACR renal domain score of 10 had significantly higher SDI renal damage scores compared with patients who had a renal domain score of 8 or 4 (both p < 0.001; Table 3). The gonadal score was also significantly elevated in patients with a score of 10 compared with a score of 8 (p = 0.001).
Table 3. Renal and gonadal SDI damage score and EULAR/ACR criteria renal domain score*
|
ACR, American College of Rheumatology; EULAR, European League Against Rheumatism; SD, standard deviation; SDI, Systemic Lupus International Collaborating Clinics/ACR Damage Index. |
|||
|
SDI domain, score (SD) |
EULAR/ACR renal domain criteria score |
||
|---|---|---|---|
|
4 (n = 74) |
8 (n = 49) |
10 (n = 173) |
|
|
Renal |
0.06 (±0.23) |
0.08 (±0.28) |
0.31 (±0.71) |
|
Gonadal |
— |
0.00 |
0.05 (±0.22) |
In a subset of patients (n = 251) who had follow-up data for ≥10 years, a trend of higher renal damage scores was seen in the ≥20 group; however, no other significant differences were noted.
The impact of LN on short term accrual EULAR/ ACR domains and SLICC/ACR damage4
Study design
This historical study included 133 patients with SLE diagnosed according to the 2019 EULAR/ACR criteria; these criteria alongside SDI were used to measure organ damage.
Patients were split into two groups depending on the presence of LN at disease onset (renal lupus, n = 49; non-renal lupus, n = 84).
Results
At baseline and at the end of the study, total domain scores were significantly higher for the renal group than the non-renal group (Figure 2).
Figure 2. Total domain score at baseline compared with the end of the study*
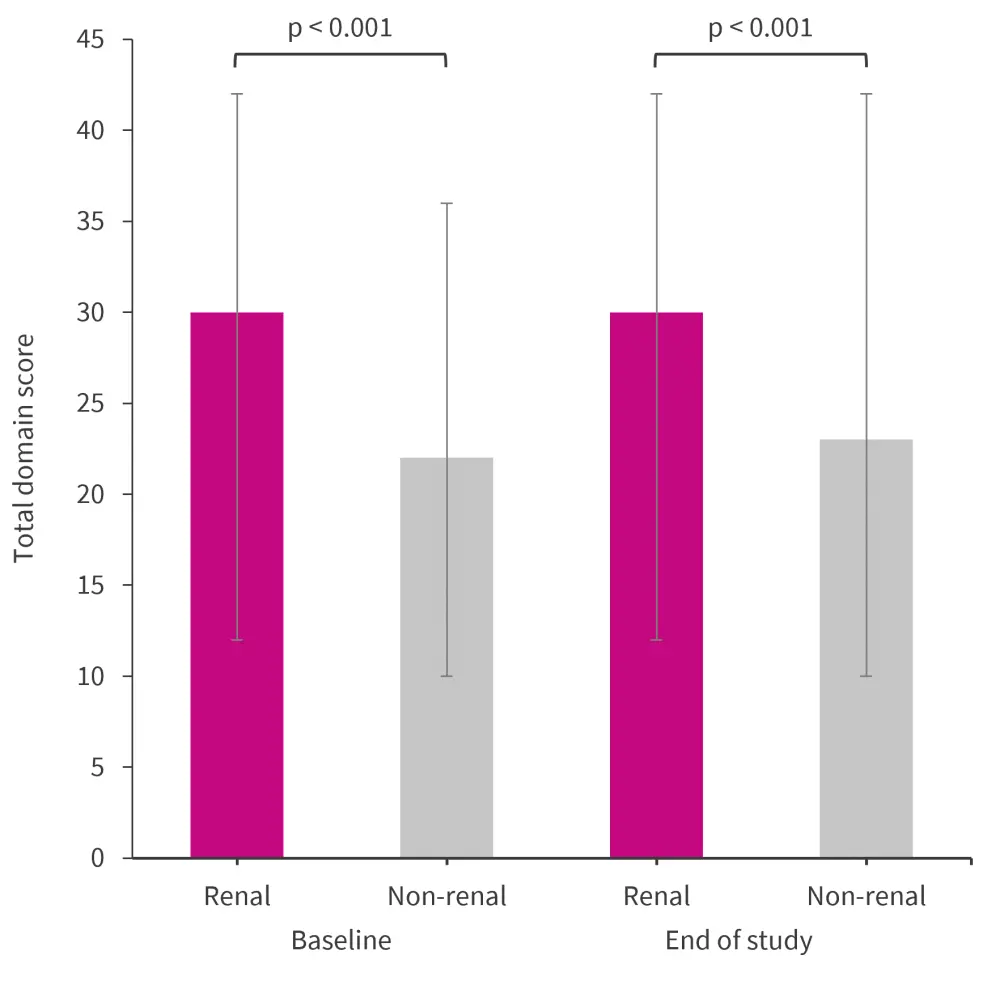
*Adapted from Munhoz, et al.4
Renal biopsies were available for 36.7% of patients with renal lupus, with the most common histological classes identified as class III/IV and II/V in 55.6% and 44.4%, respectively. There was also one case each of mixed class III-V and IV-V. Complement levels were lower in the renal group compared with the non-renal group at baseline (87.8% vs 66.7%; p = 0.007).
Total EULAR/ACR domains were stable over 3 years in the renal group, with a median total domain score at baseline and at 3 years of 30 (range, 12–42; p = 0.125); whereas the non-renal group showed a significant increase in domains compared with baseline, with a median total domain score of 22 (range, 10–36) at baseline vs 23 (range, 10–40) at 3 years (p < 0.001). Patients in the non-renal group had more cumulative new domains observed than in the renal group (44.05% vs 6.1%, respectively; p < 0.001). For patients in the non-renal group, the largest increases were seen in renal and hematologic domains (Figure 3).
Figure 3. Cumulative new 2019 EULAR/ACR domains in patients with renal-lupus and non-renal lupus after 3 years*
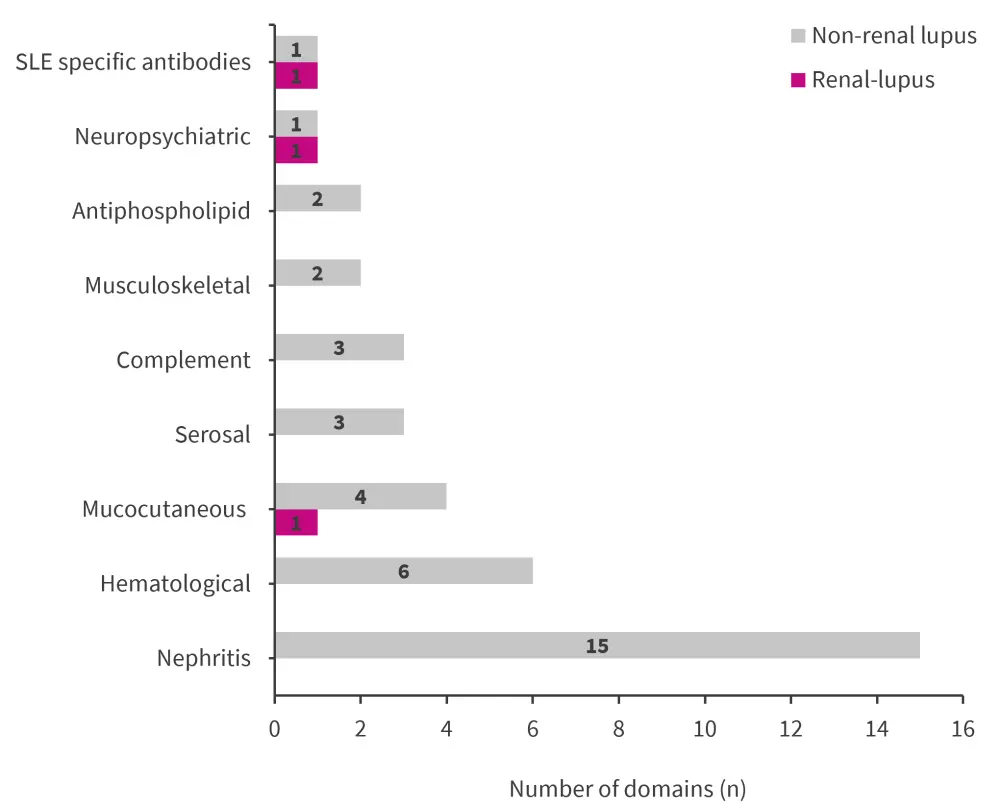
ACR, American College of Rheumatology; EULAR, European League Against Rheumatism; SLE, systemic lupus erythematosus.
*Adapted from Munhoz, et al.4
After 3 years, the renal group still had an increased prevalence of renal involvement (100% vs 17.9%; p < 0.001) and low complement levels (87.8% vs 70.2; p = 0.021) compared with the non-renal group, prevalence of the hematologic domain was also lower (51% vs 69%; p = 0.038).
Treatment
While all patients received glucocorticoids (GCs), the dose (Figure 4) and frequency of GC pulses were significantly higher in the renal group compared with the non-renal group (85.7% vs 10.7%, respectively; p < 0.001).
Figure 4. Glucocorticoid treatment and median dose at baseline and after 3 years*
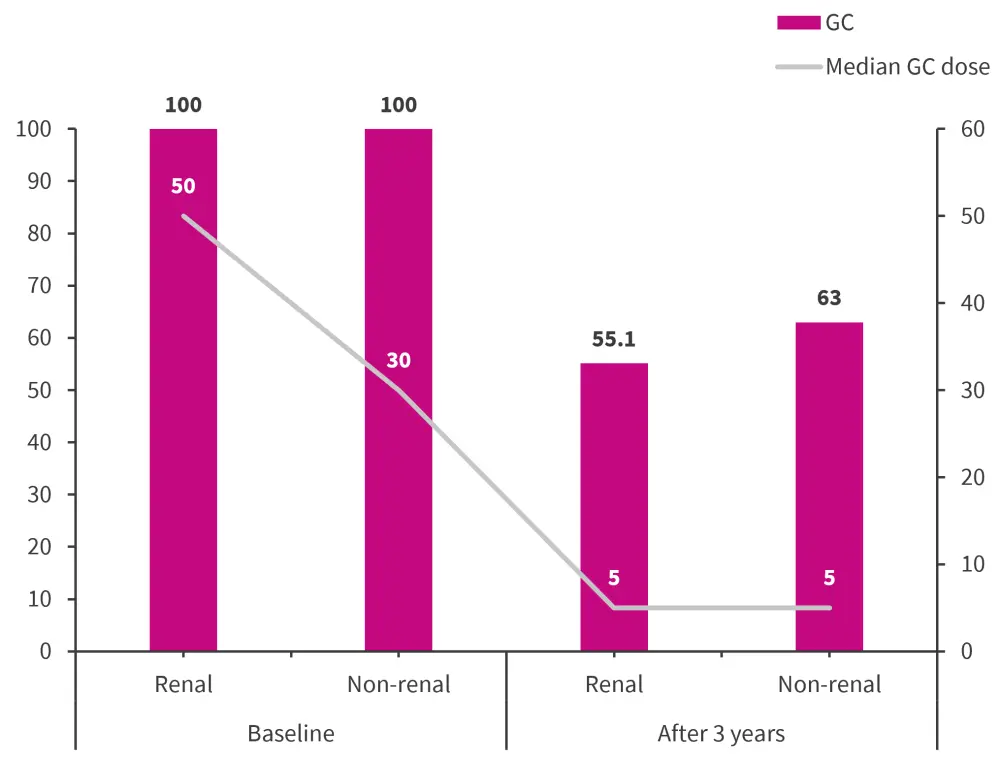
GC, glucocorticoids.
*Adapted from Munhoz, et al.4
Higher use of all therapeutic agents listed, except for azathioprine, were seen in the renal group compared with the non-renal group. After 3 years, a decrease was seen in GC use in both groups, whereas the use of mycophenolate mofetil significantly increased (p = 0.008; Figure 5).
Figure 5. Treatment at baseline and after 3 years*
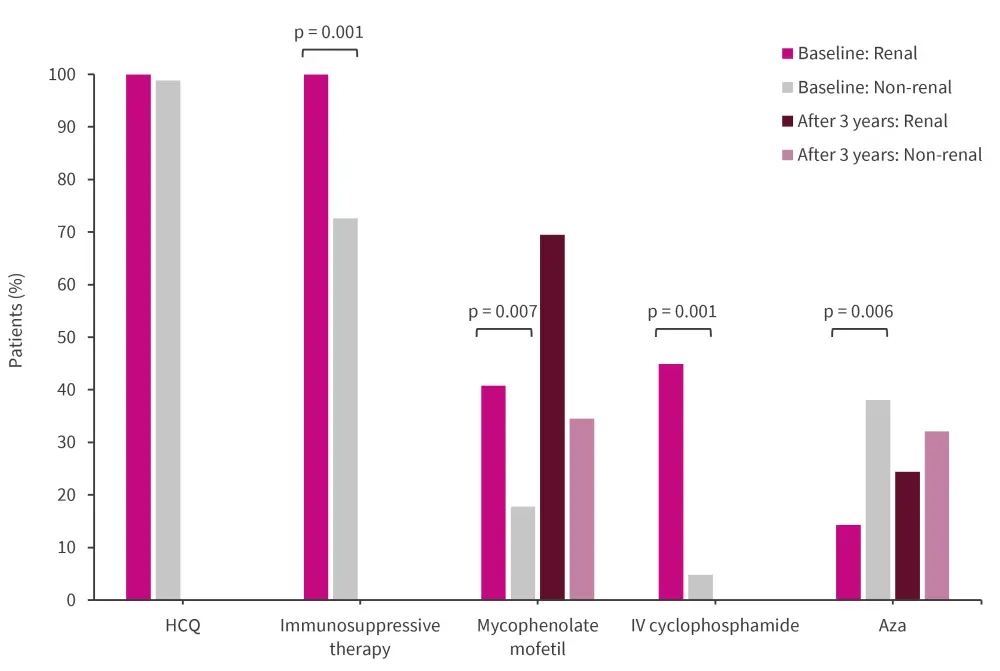
Aza, azathioprine; HCQ, hydroxychloroquine; IV, intravenous.
*Adapted from Munhoz, et al.4
Cumulative damage scores
While both the renal and non-renal groups had increased median SDI scores after 3 years, the median scores were similar between groups by the end of follow-up (1 vs 0, respectively; p = 0.132).
Both groups also showed increases in patients with SDI scores ≥1 after 3 years (renal group, 46.9%; non-renal group, 40.5%). Although the prevalence of damage was similar between both groups at 3 years, the renal group had an increased prevalence of SDI ≥2 compared with the non-renal group (22.4% vs 8.3%; p = 0.022).
By the end of the study, disease related damage was found to be higher in the renal lupus group (46.9%) compared with the non-renal lupus group (29.8%), whereas drug related damage was similar between the two groups (20.4% renal vs 14.3% non-renal). In terms of disease related damage, a significantly increased frequency of seizures was noted in the renal vs the non-renal group (6.1% vs 0%; p = 0.048).
Conclusion
Patients with EULAR/ACR scores ≥20 were found to develop significantly more organ damage than patients with scores of 10–19. The organ systems that were particularly affected include renal, cardiovascular, dermatological, and gonadal; therefore, EULAR/ACR criteria may have value as a prognostic tool, although this requires further validation.3
As discussed by Munhoz et al.,4 patients with non-renal lupus developed a significant increase in EULAR/ACR domains over the course of 3 years, particularly in the renal domain. Therefore, it is important to monitor patients with SLE who do not present with renal involvement at diagnosis for additional organ involvement within the first 3 years.
Approximately half of the patients with non-renal lupus also demonstrated a comparable increase in SDI scores, indicating organ damage compared with the renal group. This suggests that some patients with seemingly milder disease may still experience comparable levels of organ damage early on in their disease course and may require further or more intense treatment to prevent this.4
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


