All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Yeo et al. published an article in Rheumatology, analyzing the usefulness of serial anti-dsDNA monitoring in predicting the risk of flare in patients with SLE who are persistently anti-dsDNA positive.1 Here, we summarize their key results.
Methods1
- The study was conducted on the Asia Pacific Lupus Collaboration 2013–2021 dataset.
- Patients were categorized based on their anti-dsDNA results as:
- Persistently negative, who never had anti-dsDNA values above the upper limit of the normal range
- Fluctuating, who had varying anti-dsDNA results between negative and positive
- Persistently positive, who always had anti-dsDNA results above upper limit of normal range
- Anti-dsDNA results were standardized by calculating an anti-dsDNA ratio to the upper limit of normal cut-off.
- Cox regression models were used to determine the association of anti-dsDNA as a continuous variable with the risk of flare using the following two approaches:
- absolute value of anti-dsDNA ratio; and
- change in anti-dsDNA ratio from the previous visit, noted as amplitude and direction.
Key findings1
- Data from 3,484 patients with 37,582 visits were analyzed
- 92.3% were females and median age at enrolment was 39 years
- 29.5% had persistently positive anti-dsDNA, 34.3% had fluctuating anti-dsDNA, and 36% had persistently negative anti-dsDNA
- Anti-dsDNA ratio >3, as an absolute value, was significantly associated with an increased risk of flare at the subsequent visit in persistently positive and fluctuating anti-dsDNA patients with SLE (Figure 1).
- Increase and decrease in anti-dsDNA by more than 2-fold compared with the previous visit were also associated with increased risk of flare in the persistently positive and fluctuating cohort (Figure 1).
Figure 1. Cox regression analysis on association of anti-dsDNA with risk of SLE flare*
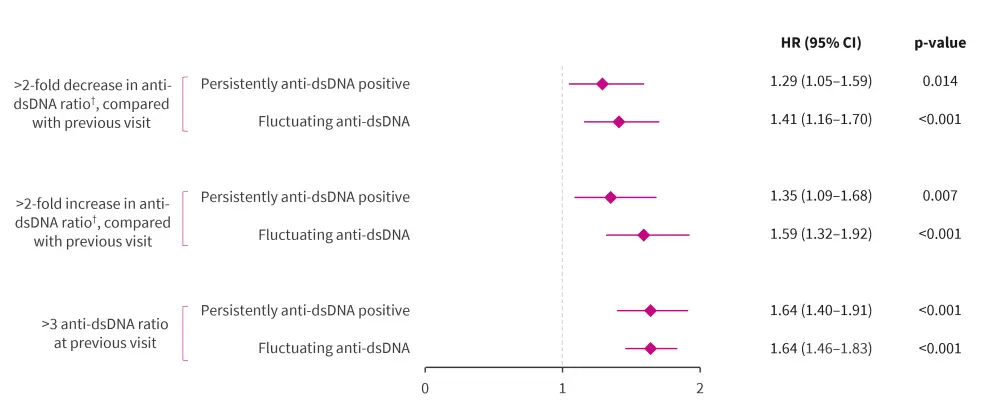
CI, confidence interval; dsDNA, double-stranded DNA; HR, hazard ratio; SLE, systemic lupus erythematosus.
*Data from Yeo, et al.1
†Calculated by taking the result divided by the upper limit of normal for that assay.
Flare was captured by using the Safety of Estrogens in Lupus Erythematosus National Assessment-SLE disease activity index.
|
Key learnings |
|
Question for expert
Expert Opinion
In recent years, there has been a growing interest in limiting the use of tests that do not significantly influence management or therapeutic decision making, to make healthcare more sustainable. In this context, some have questioned the utility of serial testing of anti-dsDNA levels in subsets of patients with SLE who persistently show positive or negative anti-dsDNA, irrespective of clinical disease activity.
Anti-dsDNA is reported on a continuous scale with a cut-off for an abnormal result. Using data from the Asia Pacific Lupus Collaboration, the world’s largest lupus cohort, there was a graded relationship between anti-dsDNA level and the risk of flare, even in patients with persistently positive anti-dsDNA, as shown in the SMART-SLE study. A two-fold increase in anti-dsDNA antibody level compared with baseline was associated with an increased risk of subsequent flare, including patients with persistently positive anti-dsDNA.
We can infer from these findings that testing anti-dsDNA level is useful in the monitoring of SLE even in patients with persistently positive anti-dsDNA, as changes in the level of this antibody provides information regarding flare risk. Future studies are needed to address the utility of measuring anti-dsDNA for lupus monitoring in patients with persistently negative anti-dsDNA and whether fluctuations in the normal range offer any clinically useful information. From a pragmatic perspective, patients with persistently negative anti-dsDNA could be a subset in which repeat anti-dsDNA testing may not be necessary outside of a research setting.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


 Mandana Nikpour
Mandana Nikpour
