All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Post-hoc analyses of phase II PAISLEY trial in patients with SLE treated with deucravacitinib
The Lupus Hub previously reported results from the phase II PAISLEY trial (NCT03252587), demonstrating the efficacy and safety of deucravacitinib vs placebo in patients with systemic lupus erythematosus (SLE). Here, we summarize several post-hoc analyses of the PAISLEY trial presented at the American College of Rheumatology (ACR) annual meeting (ACR Convergence 2023).
Key findings
- Furie et al.1 and Morand et al.2 demonstrated a shorter median time to response and higher response rate at Week 48 with deucravacitinib treatment (Figure 1A; Figure 1B).
- Arriens et al.3 showed that deucravacitinib resulted in a higher proportion of patients achieving Cutaneous Lupus Erythematosus Disease Area and Severity Index-70 at Week 48 (Figure 1B).
Figure 1. A Median time to onset of SRI(4), BICLA, dual SRI(4)/BICLA, and LLDAS response and B response rate with SRI(4), BICLA, dual SRI(4)/BICLA, and CLASI-70*
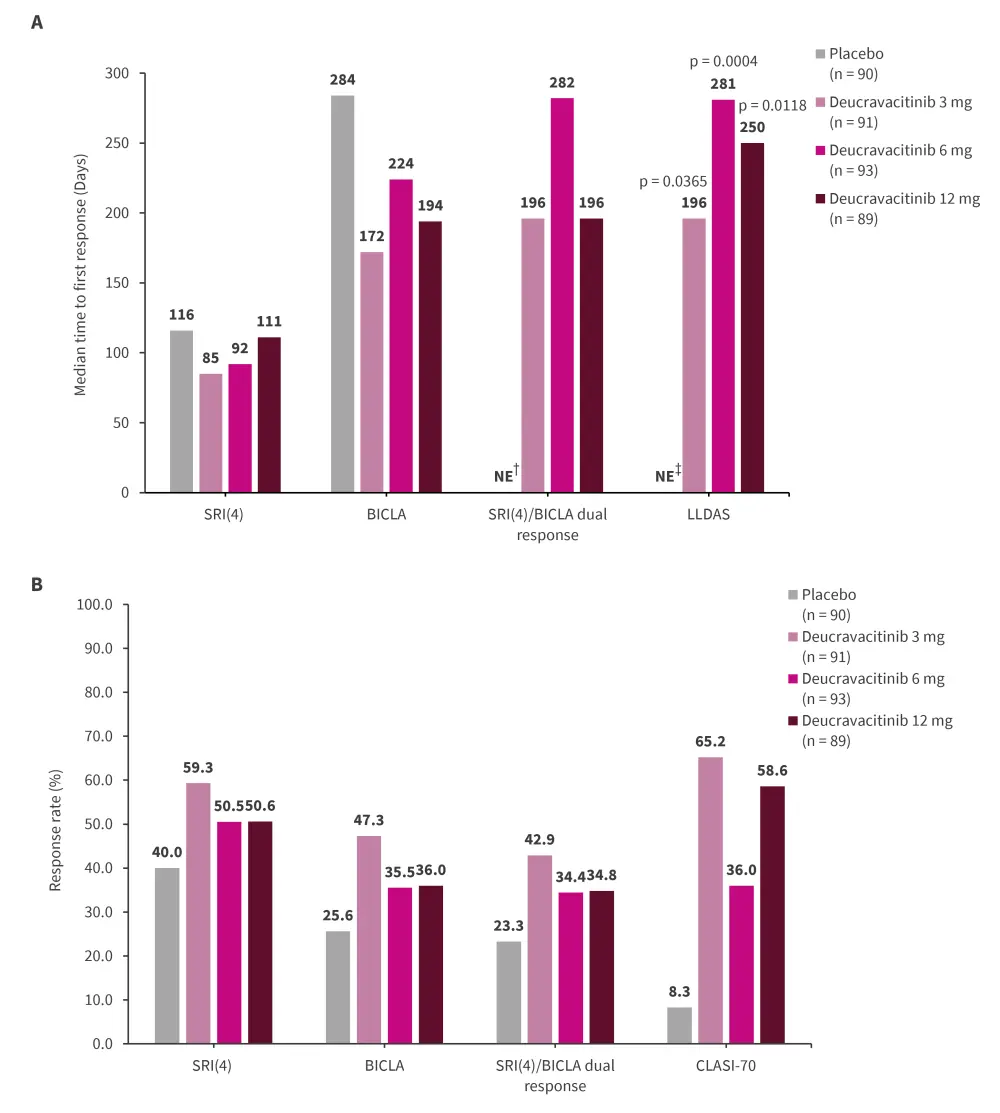
BICLA, British Isles Lupus Assessment Group–based Composite Lupus Assessment; CLASI, Cutaneous Lupus Erythematosus Disease Area and Severity Index; LLDAS, Lupus Low Disease Activity State; NE, not estimable; SLE, systemic lupus erythematosus; SRI(4), SLE Responder Index-4.
*Data from Furie, et al.1; Morand, et al.2; and Arriens, et al.3
†Because they exceeded the period of the study (48 weeks/336 days).
‡Due to a less than 50% probability of achieving LLDAS at any time point.
Transcriptomic analysis by Wu et al.4 revealed that:
- Patients with SLE expressed higher levels of interferon (IFN)-regulated genes, including IFIT1 (interferon-induced protein with tetratricopeptide repeats 1) and interferon induced protein 44, which were significantly reduced following treatment with deucravacitinib.
- CMPK2 (cytidine/uridine monophosphate kinase 2) and interferon induced protein 44 appear to be particularly relevant to SLE pathophysiology.
Further, a novel IFN 5 gene (MX1 [MX Dynamin Like GTPase 1], HERC5 [HECT and RLD domain containing E3 ubiquitin protein ligase 5], IFIT1 [interferon-induced protein with tetratricopeptide repeats 1], RSAD2 [radical S-adenosyl methionine domain containing 2], and EIF2AK2 [eukaryotic translation initiation factor 2 alpha kinase 2]) signature was developed by Wu et al.5 to classify patients with SLE into IFN high or IFN low subgroups. Pharmacodynamic analysis revealed that deucravacitinib:
- Reduced IFN 5 gene score and anti-double stranded DNA antibody titers in both groups.
- At Week 32, higher SRI(4) was observed with a dosage of 3 mg twice daily and 12 mg once daily, along with an increased British Isles Lupus Assessment Group–based Composite Lupus Assessment response rate at Week 48.
Mosca et al.6 assessed patient-reported outcomes and revealed that deucravacitinib achieved clinically meaningful improvements (meeting or exceeding minimal clinically important/minimally important differences) in pain, fatigue, and health-related quality of life from baseline at Week 48 (Figure 2).
Figure 2. Patient-reported outcome measures in post-hoc analysis of the phase II PAISLEY trial*
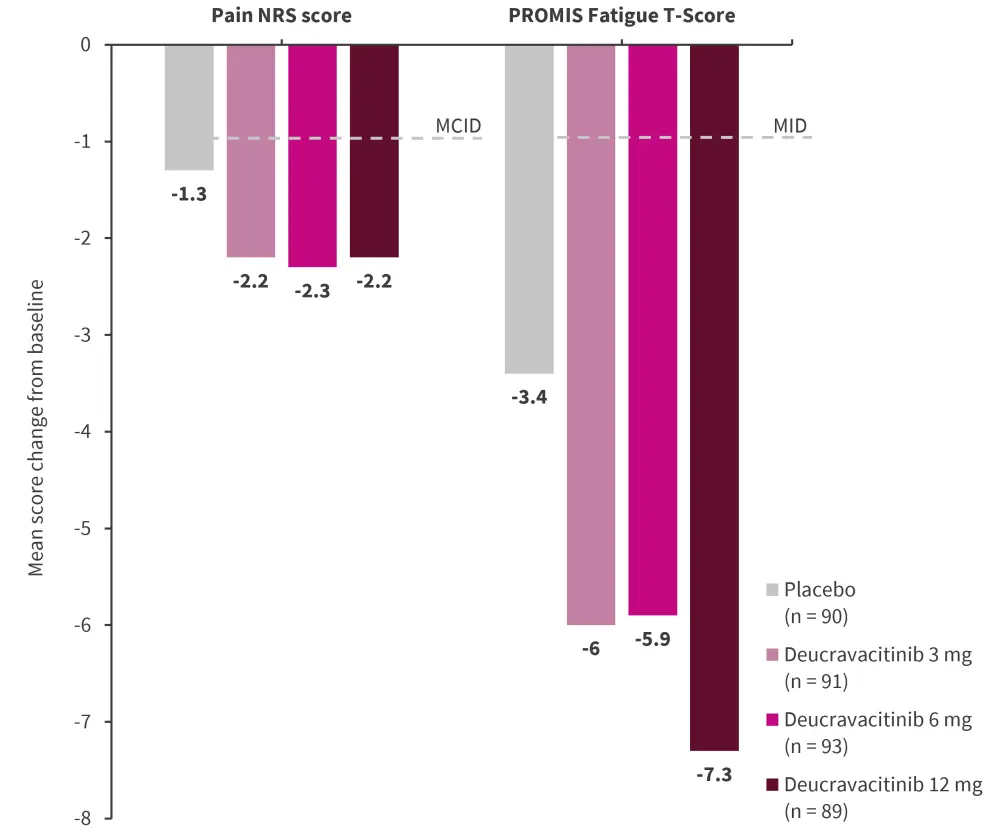
MCID, minimal clinically important difference; MID, minimally important difference; NRS, numeric rating scale; PROMIS, Patient-Reported Outcomes Measurement Information System.
*Adapted from Mosca, et al.6
|
Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content



