All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional.
The lupus Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lupus Hub cannot guarantee the accuracy of translated content. The lupus and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lupus Hub is an independent medical education platform, supported through a founding grant from AstraZeneca. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lupus content recommended for you
Link between severe non-adherence to hydroxychloroquine and SLE flares: SLICC cohort study
Featured:
The effectiveness of hydroxychloroquine (HCQ) is known to decrease with non-adherence (reported range, 3–85%) in patients with systemic lupus erythematosus (SLE). Here, we summarize the Systemic Lupus International Collaborating Clinics inception cohort study examining the association between severe non-adherence to HCQ and SLE flares, published by Nguyen et al.1 in Arthritis and Rheumatology.
Methods1
In this international multicenter cohort study, serum of 660 patients receiving HCQ for at least 3 months was analyzed.
- Serum HCQ levels of <53 ng/mL or <106 ng/mL for HCQ doses of 200 mg or 400 mg/day, respectively, were defined as severe non-adherence.
- SLE flare was defined as an increase of ≥4 points in SLE Disease Activity Index 2000, use of prednisone or immunosuppressive drugs, or new renal involvement in the first year after time zero (T0).
- SLE damage was defined as an increase of ≥1 point in Systemic Lupus International Collaborating Clinics Damage Index.
Key findings1
- Overall, 7.3% of the patients included were severely non-adherent to HCQ.
- HCQ levels of <53 ng/mL and <106 ng/mL were seen in 7.7% and 7.1% of patients receiving HCQ doses of 200 mg and 400 mg/day, respectively.
- The median serum HCQ was 388 ng/mL (interquartile range [IQR], 244–566 ng/mL).
- The median HCQ levels were 250 ng/mL (IQR, 158–365 ng/mL) and 427 ng/mL (IQR, 287–602 ng/mL) for HCQ doses of 200 and 400 mg/day, respectively.
- In the univariate analysis:
- Severe HCQ non-adherence (odds ratio [OR], 3.86), age (OR, 0.98), SLE Disease Activity Index 2000 (OR, 1.06), and treatment with azathioprine at T0 (OR, 1.95) were associated with an increased risk of SLE flares.
- Black race (OR, 1.59), education (OR, 2.02), smoking (OR, 1.52), body mass index (OR, 1.03), treatment with azathioprine at T0 (OR, 2.01), and non-quantifiable serum HCQ level (OR, 1.99) were associated with an increased risk of SLE damage.
- Severe HCQ non-adherence (hazard ratio, 5.41) was associated with a risk of death during the 5 years after T0.
- Figure 1 shows the multivariate analysis of factors associated with SLE flare and damage.
Figure 1. Multivariate analysis of factors associated with SLE flare and damage*
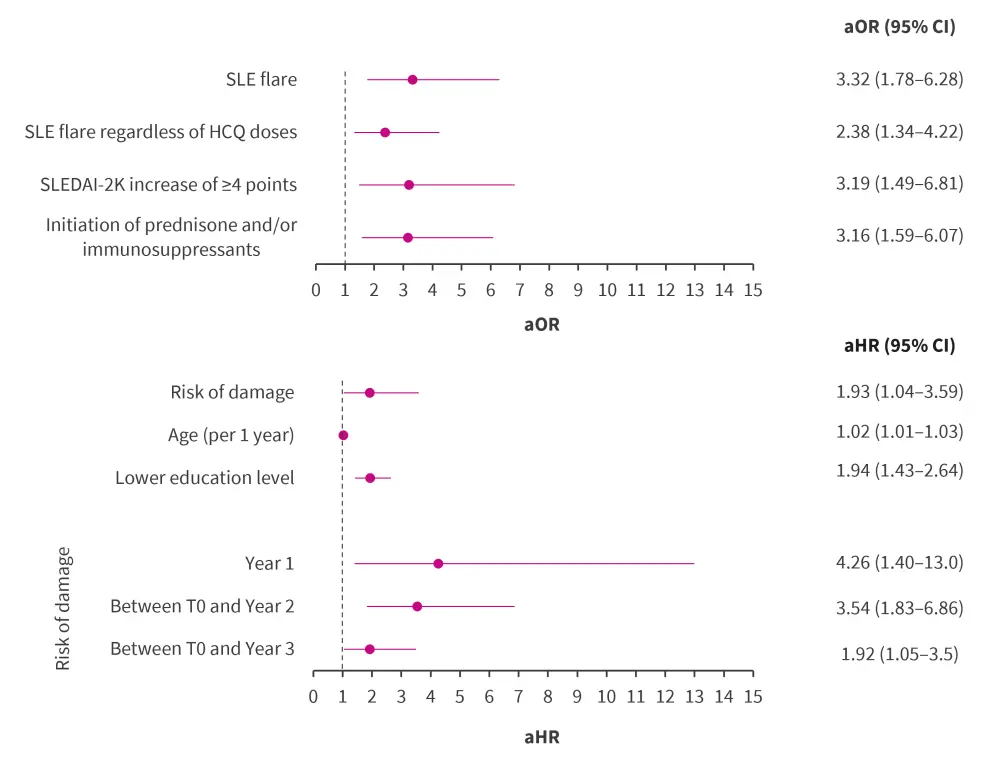
aHR, adjusted hazard ratio; aOR, adjusted odd ratio; CI, confidence interval; HCQ, hydroxychloroquine; SLE, systemic lupus erythematosus; SLEDAI-2K, SLE Disease Activity Index 2000 index; T0, time zero.
*Data from Nguyen, et al.1
|
Key learnings |
|
Question for expert
Expert opinion
This study demonstrates that non-compliance, measured by severe HCQ non-adherence, is associated with poor outcomes. This should prompt clinicians to better understand the causes of non-adherence and develop approaches to address them. In a previous study,2 we have demonstrated that non-compliance in at least 50% of patients is due to: concerns about harmful side effects, being easily distracted, life getting in the way, being unsure or disagreeing that their condition will worsen without medications, and personal reasons. Each of these patient concerns can be addressed through remedial approaches by physicians and other healthcare professionals treating patients with lupus.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


 Murray Urowitz
Murray Urowitz
